World Nutrition
Volume 3, Number 8, August 2012
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary: Food supplies. Trans-fats
Government policies and actions
to protect citizen health

Vivica Kraak
WHO Collaborating Centre for Obesity Prevention
Deakin University, Victoria, Australia
Biography posted at www.wphna.org
Email: vivica.kraak@deakin.edu.au
Access pdf of linked July commentary here
Introduction
Editor's note
In this commentary Vivica Kraak reports on some of the policies and actions of governments in four countries that have been designed to improve the nutritional quality of food supplies, and thus protect against obesity, cardiovascular disease and other chronic non-communicable diseases. She pays special attention to government initiatives in Denmark and the United States, which have used a combination of voluntary and legal approaches, and compares these with Australia and England, whose governments have relied heavily upon voluntary approaches. She also reports on work being done by colleagues at the University of Oxford, who recommend that governments use fiscal policies, including taxes, both to influence citizens' food choices and to raise revenue for obesity prevention or public health programmes.
The commentary takes an unusual form. It is conventionally researched, analytical, and fully referenced. It also is a story of a professional and personal journey across three continents, in which the reporter is present throughout. In this way it reminds us that policies are observed, made and shaped by people.
Stimulated by a recent visit to Denmark, the first country in the world to ban trans-fatty acids from the food supply (in 2003), and to pass a law taxing saturated fats (in 2011), in this commentary I explore the world of restrictions, taxes and bans on 'substances of concern' including unhealthy food and drink products. I focus on how trans-fat reduction and removal have been pursued in four countries across three continents that I visited during 2012. This has led to some surprising discoveries about how governments are combining both soft (voluntary) and hard (statutory) policies whose purpose is to improve the nutritional quality of food supplies, in order to reduce peoples' consumption of unhealthy foods, drinks, nutrients and other edible substances.
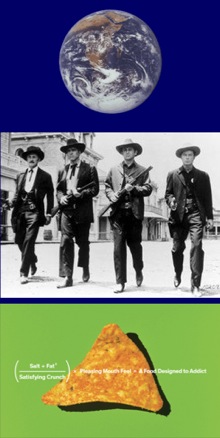
Some scholars call the foods identified here as 'of concern', by the acronyms HFSS (high-fat, salt or sugar) or SOFAS (high in solid fats and added sugars, one category being SSB (sugar-sweetened beverages).Others take a broader and less technical view and refer to highly refined, or high energy-dense, or low nutrient-dense, or ultra-processed snacks, products, foods, meals, or dietary patterns. The US food writer Michael Pollan uses the term 'edible food-like substances' (1).
Whatever the preferred concepts or terminology, the evidence is very clear that the whole world's population is rapidly shifting to dietary patterns in which the majority of people are consuming far too many unhealthy foods and drinks within energy-dense diets, and are also increasingly sedentary. For reasons that have been covered in many other World Nutrition commentaries, most people now do not consume adequate varied nutrient-dense diets, summarised in seven simple words by Michael Pollan as 'Eat food. Not too much. Mostly plants' (1).
Policy entrepreneurs may perhaps think that the insights here are self-evident and intuitive. But real-life case studies are useful to inform similar efforts in other countries to reduce saturated fats, added sugars, salt, and energy-density in their food supplies, while improving the nutritional profile of foods and nutrient-density of people's regular diets, in order to prevent and control obesity, and to reduce the rates of chronic non-communicable diseases.
In this commentary I do not examine the nature and extent of resistance to change. These include the lobbying and political pressures put by food and drink product manufacturers and industry trade groups on policy-makers, to block or oppose policies intended to protect and promote public health which threaten commercial interests. I also do not explore policy approaches to create physical environments that promote physical activity.
Rather, I explore examples of when governments have used soft or hard policies, or combined these approaches, to improve both the quality of dietary patterns and food supplies. My sleuthing started in Denmark. I sought to understand how the trans-fat ban evolved. Then I briefly compare how trans-fat reduction has been pursued in three other countries (Australia, England and the United States) on three different continents (Oceania, Europe, North America).
Trans fats
From soft to hard policies and actions
Nearly 20 years ago, worldwide media attention spotlighted a study published in the Lancet by Association founder member Walter Willett and colleagues from the Harvard School of Public Health. Its topic was the relationship between trans-fat consumption and coronary heart disease (2). The study's conclusion was couched in cautious language but the message got across. 'Intakes of foods that are major sources of trans isomers (margarine, cookies [biscuits], cake, and white bread) were each significantly associated with higher risks of CHD. These findings support the hypothesis that consumption of partially hydrogenated vegetable oils may contribute to occurrence of CHD'.
This study and a vast amount of subsequent research (3), show that trans-fats are harmful to human health. They raise the 'bad' total and low-density lipoprotein cholesterol levels and reduce the 'good' high density lipoprotein cholesterol, thereby increasing risk of cardiovascular disease. They are found in processed products that contain hydrogenated or partially hydrogenated vegetable fats, including a great range of fried and baked goods. Food manufacturers have used the hydrogenation process to generate trans-fats for almost a century, at first notably in harder margarines, then in an increasingly vast range of baked, fried and otherwise processed products and packaged snacks, to extend the stability and shelf life of their products.
 Trans fats: Denmark's experience
Trans fats: Denmark's experience
Restrictions in the public interest

First stop Copenhagen. Here is a pedestrian street at the Nyhavn Canal (left) and here I am with Gitte Laub Henson of the Danish Cancer Council (right).
The seed for this commentary was sown during a visit to Denmark in early June. I had been invited to speak at a conference hosted by Aalborg University in Copenhagen that explored the conditions for fostering constructive government, industry and civil society partnerships for healthy eating. This wasn't my first trip to Copenhagen. Each visit, I take in the city's historic beauty, meet its friendly people, and experience the signature Nordic cuisine and active transport culture.
At the conference, I learned that Denmark was the first country in the world to pass a substantial tax on saturated fats, in December 2011 (4), and that it is currently considering passing a sugar tax. The fat tax law has two purposes. The first is to discourage Danes from consuming excessive amounts of milk, butter, cheese, meat and highly processed products high in saturated fats, to reduce their cardiovascular disease risk. The second purpose is to generate revenue to meet a budget shortfall. This was not the first time that the Danish government had successfully passed a food policy tax for its 5.5 million citizens.
The Danish ban on trans-fats
While in Copenhagen, I visited my Danish colleague Gitte Laub Hansen (see above). She was a member of the Danish Nutrition Council that reviewed the evidence on the relationship between industrially-generated trans-fats and cardiovascular disease risk in the early 1990s. She and others told me that while experts in Denmark's public health community had been concerned about trans-fats in their food supply since the 1980s, the international media blitz was a tipping point for the country. In 1993, Denmark's government initiated trans-fat reduction through voluntary collaborations with industry to remove trans-fats and to reformulate processed food products (5).
A subsequent Danish Nutrition Council report released in 2003 (6) concluded that trans-fats are associated with a 10-fold higher risk of developing cardiovascular diseases. A decade after it had embarked on the voluntary approach to reduce trans-fats in the food supply, Denmark became the first country in the world to adopt legislation to ban trans-fats in foods (7).The regulation was driven by many converging and diverse interests, and actions and interactions among food companies, public health nutrition experts and policy-makers. The story is told in a fascinating case study published by colleagues at Aalborg University (5).
Since Denmark trades with other European Union countries, the EU challenged the trans-fat ban. This precipitated a lengthy policy negotiation process. Denmark's decision influenced other countries to follow its lead, and several EU member states (Austria, Switzerland and Iceland) also banned trans-fats from their food supplies. By 2007 the EU accepted the evidence that justified the Danish ban. This may have also influenced the recommendation of the joint WHO/FAO report released in 2008 that trans-fats should not exceed 1 per cent of total calories consumed per person per day (8).
The Danish government has monitored the level of trans-fat in the national food supply. Results suggest that only 7 per cent of the tested products have more than 2 grams of trans-fat per 100 grams of fat, a majority of which are of foreign origin (Hansen GL, personal communication, June 2012).
More recently, the Danish government has been asked by industry trade associations and also trades unions to abandon the fat and proposed sugar tax, due to cross-border shopping for less expensive food products purchased by Danish consumers, which are implicated in economic revenue and job losses (9). No decision has yet been made to reverse the law.
 Trans fats: The US experience
Trans fats: The US experience
Voluntary and statutory measures
In the US, any development or change in food systems and supplies is made in collaboration with industry and other vested groups, including public-interest non-government organisations. Since the early 1990s the Center for Science in the Public Interest (CSPI), the Washington-based consumer advocacy group, had been petitioning the US federal government and the US Food and Drug Administration (FDA) to require trans-fat to be listed on the Nutrition Facts panel that appears on the labels of most processed food products. The FDA had encouraged food manufacturers to reduce trans-fats in products including baked goods, chips (crisps), other snack foods, and pre-prepared meals, dishes and desserts, but then eventually in January 2006, the FDA made trans-fat disclosures mandatory on the 'Nutrition Facts' panel. CSPI director Michael Jacobson, who calls trans-fat 'the single most harmful fat in our diet,' notes that it took the FDA 13 years to respond to the CSPI request (10).
Preliminary findings published in 2012 suggest a 58 percent decline in trans-fats in the blood of US people between 2000 and 2009 (11). A US Department of Agriculture (USDA) report has also found a substantial decline in the trans-fat content of new food products marketed from 2005 to 2010, accompanied by an increase in the use of 'no trans fats' nutrition health claims on product packages (12).
In a Journal of the American Medical Association invited editorial published in July (this month as I write), an evaluation conducted by the FDA is cited. This estimates that the average consumption of industrially produced trans-fats in the US has decreased from about 4.6 grams per person per day (2.0 per cent of energy) in the late 1990s to about 1.3 grams per person per day (0.6 per cent of energy) by 2010. A majority of the food products examined by the FDA now contain less than 0.5 grams of total trans-fat per serving. Population averages however conceal groups that consume higher levels: 10 per cent of US residents aged 2 years or older consume more than 2.6 grams per person per day of industrially produced trans-fat (13).
The reduction of trans-fats in the US food supply can be partly attributed to the government combining soft and hard policies: in this case, food manufacturers' voluntary reformulation of products, together with the mandatory labelling disclosure stimulated by consumer advocacy and public health groups. The USDA report found that new products without trans-fats also generally contained less saturated fat, sodium and calories, which suggests that product reformulation has moved in a generally healthier direction.
Do these changes go far enough? The invited editorial (13) recommends elimination of partially hydrogenated oils, the main source of industrially-generated trans-fats in processed and restaurant foods consumed frequently by people eating out of home in all packaged foods, and foods prepared and sold in restaurants and other food service outlets. Likewise, CSPI recommends that the FDA initiates and implements a national ban on partially hydrogenated oils (14).
New York was the first US city to ban the use of artificial trans-fats by restaurants and catering outlets, in 2006 (15). The state of California and the cities of Philadelphia and Baltimore have followed New York City's lead. (I have more to say below about New York City's policies and actions since 2002, when Michael Bloomberg was elected Mayor). These state or city bans specify an upper limit of 0.5 grams of trans-fats per standard serving of a processed food or a restaurant meal, which can however add up to quite a substantial daily intake.
The city of Cleveland, concerned about trans-fats, in 2012 fought and won a legal battle against Ohio state legislators who passed a law in 2011 to prevent local governments from banning restaurants from using cooking oils that contained trans-fats. Overruling this law in favour of Cleveland in 2012, a county judge ruled that the state law was an improper attempt to stop the city from exercising its home rule power (16).
The combination of soft and hard policy measures used in the US needs to be interpreted in the context of a country whose culture is deeply individualistic and generally adverse to government interventions. See Box 1.
Box 1
Most people don't support taxes and bans
The words 'restrict', 'tax', and 'ban', tend to generate visceral responses from people across different countries and cultures. This is despite the fact that when enacted, laws such as those that restrict parking, tax cigarettes, ban driving without seat-belts, encourage recycling, and provide universal health care coverage, become accepted over time. As defined here:
A restrictionis a regulation or law that limits or controls choices.
A taxis a fee charged by government on a product, income or activity, serving as a way for society to redistribute wealth and services (for example, education and health to benefit everyone) and support the infrastructure for society to function properly (for example, to build or repair roads and support civil services).
A ban involves prohibiting or forbidding, particularly through official means to promote health, protect the environment, and protect the well-being of vulnerable groups such as children and adolescents.
A recent global survey conducted among 18,500 adults in 24 countries (17) has explored peoples' acceptability of government interventions for several policy issues, including measures that restrict unhealthy eating. There is broad variation across countries. But half of the respondents generally said that governments should not be involved in influencing peoples' dietary choices. Legislators know that policies without broad public support are less likely to succeed. That is why governments listen to public opinions and the positions of interest groups when considering behavioural change legislation that ranges from nudging to shoving.
Consideration of food and drink restrictions, taxes and bans raise several important questions. For example:
- When and how should governments include such measures to halt and reverse costly obesity and chronic non-communicable disease epidemics?
- What is a reasonable goal and time-frame to improve the quality of food supplies? Fifty or even 20 to 25 years is too long to wait.
- What previous food policy successes and failures show how best to create and sustain healthy food and eating environments?
 Trans fats: The Australian experience
Trans fats: The Australian experience
Reformulation and education

Second stop Melbourne. Here is the Eureka building in the centre of the city
(left); and (right) here I am ,with graduate students at Deakin University
Individualism, and scepticism about government intervention, are features of Australian culture. In contrast to the US, approaches to reduce trans-fats in Australia have relied primarily on partnerships and collaborations among various vested groups to reduce trans-fats in the food supply.
In 2007 the Australia New Zealand Collaboration on trans Fats was established as a public-private partnership between representatives from the National Heart Foundation of Australia, the National Heart Foundation of New Zealand, the Dietitians Association of Australia, the Australian Food and Grocery Council, the New Zealand Food and Grocery Council, the New Zealand Food Safety Authority (NZFSA) and the government agency Food Standards Australia and New Zealand (FSANZ). This collaboration promoted industry and public health initiatives to reduce trans-fats in the food supply and to increase consumer awareness and understanding. As a result, food manufacturers can voluntarily disclose the trans-fat content of their products, unless they make a nutrition claim about a product, in which case the disclosure is mandatory.
The Roundtable on trans Fats in the Quick Serve Restaurant Industry was established to reduce the trans-fat content of fast foods. It found that most companies had voluntarily reduced trans-fats in foods to what were regarded as acceptable levels (18). A FSANZ review in 2009 found that non-regulatory measures were effective in reducing trans-fats in Australia's food supply, and attributed this to voluntary initiatives of the food industry. The Australia and New Zealand Food Regulation Ministerial Council concluded in 2009 that pursuing a non-regulatory approach for this specific substance of concern was adequate but should be monitored (19).
In 2010 FSANZ reported that Australians consume about 0.5 percent of their daily energy from trans-fats, well within the WHO recommendation of less than 1.0 percent. The report also stated that about 60-70 per cent of trans-fats in the Australian diet is not from industrially produced but from natural sources, primarily derived from meat and other animal products (20). The implication is that the authorities in Australia and New Zealand do not currently view trans-fats as a major public health threat, compared with the need for reducing rates of obesity and of cardiovascular and cerebrovascular disease, linked with peoples' regular and excessive consumption of nutrients of concern such as fat, added sugars, and salt.
 Trans fats: The English experience
Trans fats: The English experience
Nudging instead of shoving
In England, calls to reduce trans-fats in processed products and to initiate explicit and then mandatory product labelling have been made since the 1990s and into the 2000s (21). In 2010, the National Institute for Health and Clinical Excellence (NICE) released a report that outlined 12 comprehensive recommendations for reducing cardiovascular disease risk among UK citizens (22). The report concluded that trans-fats are a significant health hazard to the population, especially for certain groups, such as socially disadvantaged people living on fixed or low incomes, who regularly consume fried, baked, and other processed fast foods.
The NICE report recommended six actions for the UK government to lead and coordinate:
- Eliminate the use of artificial trans-fats use for human consumption.
- Introduce legislation to ensure that trans-fats levels do not exceed 2 per cent in fats and oils used in food manufacturing and cooking.
- Direct the bodies responsible for national surveys to measure and report on consumption of trans-fats by different population subgroups, rather than only by mean consumption across the entire population.
- Establish guidelines for local authorities to independently monitor trans-fats levels at restaurants using existing statutory powers.
- Create and maintain conditions at national and local levels to support a reduction in trans-fats and prevent their replacement with saturated fats, while encouraging the use of vegetable oils high in mono- or polyunsaturated fats.
- Develop UK-wide guidelines and information for the food service sector and local government to remove trans-fats from the food preparation process, which can be used to support legislation that can be implemented throughout the UK to reduce trans-fats.
By the end of 2011, most relevant food companies had voluntarily removed trans-fats from their products or else had signed pledges to do so. This was at first through government-industry-non government organisation partnerships facilitated by the UK Food Standards Agency and other groups. More recently, further progress has been encouraged by the Department of Health through the Public Health Responsibility Deal Food Network pledges, using the 'nudge' approach (23).
By 2012, the government has not yet addressed the comprehensive approach to trans-fat removal recommended by the 2010 NICE report. Which?, a leading UK consumer organisation, conducted an evaluation on trans-fat in England (24), and in March 2012 recommended that further progress could be made if the UK government banned industrially-generated trans-fats completely. One outcome of a ban would be that smaller companies, takeaways, caterers, restaurants and others who have not signed up to the Responsibility Deal trans-fat pledge would be compelled to remove the substance from their products. In the current political and economic climate, statutory measures taken by the UK government are highly unlikely.
Statutory and fiscal policies
Taxation in the public interest

Third stop Oxford. The Radcliffe Camera Library (left); and (right) Mike Rayner, me, Oliver Mytton in the university's Department of Public Health
I have been based at the University of Oxford in England since May 2012. My task is to research stakeholders' perceptions about accountability processes and mechanisms for the Public Health Responsibility Deal Food Network. My colleagues Mike Rayner and Oliver Mytton (pictured above), work in the Department of Public Health at the university's British Heart Foundation Health Promotion Research Group. They recently published a commentary in the British Medical Journal (25) that provides a rationale for governments using fiscal measures to improve public health outcomes.
Many different terms are used to describe health-related food taxes, which can be used to reduce peoples' consumption of unhealthy substances and products, or to generate revenue that may be used to support public health programmes. The Oxford Health Promotion Research group recommends using an inclusive term, 'health-related taxes', instead of the rather negative terms, 'fat tax' or 'sin tax', as a guide for governments to justifiably use fiscal measures such as taxes. The group also describes the circumstances under which people are more willing to accept these fiscal measures.
They propose that health-related taxes are justified when the 'marketplace' fails to provide the optimum amount of a 'good' (such as healthy foods and drinks) to support society's well-being. Though evidence is mixed, people are more likely to support taxes when governments earmark them for public health initiatives such as smoking cessation or childhood obesity prevention programmes (25, 26) rather than for more general purposes such as roads and infrastructure. The Oxford Health Promotion Research group states that health-related taxes are more likely to be effective when:
- Taxes are placed on a wide range of unhealthy foods or dietary substances in order to produce greater health benefits than would accrue from narrow taxes from food groups or food items.
- Taxes need to be at least 20 percent over the product's untaxed price in order to significantly reduce obesity and cardiovascular disease rates.
- Taxes on unhealthy foods should ideally be combined with subsidies on healthy foods such as vegetables and fruits.
Public health policies and actions
Governments: responsible and accountable
There are degrees of public support for government legislation designed to influence and change food environments and eating behaviour. Government interventions can range from 'nudging' to 'shoving'. Research suggests that countries with an authoritarian culture and top-down government structures are more likely to support restrictions, whereas countries with an individualistic culture whose governments favour the 'free market' are less likely to favour 'hard' types of intervention such as taxes and bans (17).
The Nuffield Council on Bioethics (27) has developed an 'intervention ladder' that specifies a hierarchy of government interventions (Figure 1). Each successive step on the ladder involves a greater degree of intervention and higher political risk but can provide more benefits for entire populations. This is a useful way to organise thinking and discussion.
Legislators are keenly aware that public support is crucial for higher levels of intervention. Arguably, they have untapped opportunities to shape underlying social norms and attitudes to generate public support for hard policy measures that are intended to protect and promote health. They can initiate a range of interventions by simultaneously pursuing steps 1-5 in order actively to promote nutrient-dense diets, and also steps 6-8 to discourage dietary behaviours that lead to peoples' excessive consumption of highly processed, nutrient-poor and energy-dense diets.
Figure 1
The intervention ladder. How many steps?
Government actions to create healthy food and eating environments Adapted from (27)

The 'intervention ladder' is a way to classify actions that governments can take to improve public health nutrition outcomes. The bottom steps are politically easy and least effective. The higher steps are more challenging, especially when powerful opponents criticise them as attacks on people's right to choose, but they are often the most effective for improving public health nutrition outcomes.
Step 1.At the bottom of the ladder. This is the safest political move. Governments do nothing, or only monitor a public health crisis.
Step 2. This provides information to guide peoples' choices through health education or social marketing campaigns.
Step 3. This involves alliances or collaborations which for example encourage industry to change processing, such as product reformulation, or marketing practices. These changes may be unknown to or not perceived by consumers.
Step 4. This intervenes, for example, by making fresh fruit or vegetables preferred side dishes instead of french fries (chips), and non-caloric drinks such as water the preferred drinks instead of sugary products, in worksite canteens and schools.
Step 5. This encourages healthy decisions by offering manufacturers tax breaks for reformulating products or for making pledges to improve their product ranges; or subsidising healthy foods; or undertaking well-funded and sustained social marketing campaigns to change purchasing and eating habits over time.
Step 6. This discourages healthy decisions, for example, by passing taxes on energy-dense and nutrient-poor products, or by making unhealthy products unappealing by use of counter-advertising campaigns.
Step 7.This involves statutory legislation whose purpose is to reduce unhealthy ingredients, including salt, fat, added sugars and trans-fat, from specific food or drink products or in the overall food supply.
Step 8.The top of the ladder is the strongest level of government intervention. This step involves passing legislation designed to eliminate unhealthy products, for example by prohibiting trans-fats in food products or preparation, or not allowing supersized sugary drinks to be sold in public places. These types of policy interventions are the most effective and broad in their impact on public health nutrition goals.
 USA
USA
The Bloomberg factor in New York City

New York City and the Statue of Liberty (left); and (right): Mayor Bloomberg explains why the City is banning supersized portions of sugared soft drinks
The firm measures taken in Denmark are small compared with what continues to happen in New York City with multibillionaire Michael Bloomberg as Mayor since 2002.
As a US citizen living abroad, I have followed with great interest the media coverage of public health debates about proposals for taxes on sugared soft drinks or SSB (sugar-sweetened beverages). There is an abundance of evidence and strategies initiated by consumer and public health advocates to champion a tax to raise revenue and reduce their consumption (28, 29). These actions have been met with resistance and powerful counter-strategies mounted by well-funded corporations and industry group allies, with the purpose of reframing the public discourse to oppose any form of restriction, taxation or ban.
The national mood is shifting. In May 2012, an expert committee convened by the Institute of Medicine of the US National Academies, under the auspices of a Standing Committee on Childhood Obesity Prevention chaired by Association member Shiriki Kumanyika, released a report funded by the Robert Wood Johnson Foundation (30). The report emphasises that 'Currently, two-thirds of American adults and nearly one-third of American children are overweight or obese, and obesity-related illness costs the nation an estimated $190.2 billion per year... These staggering human and economic costs, along with the difficulties of treating obesity and the slow progress made in reversing national obesity trends, underscore the urgent need to accelerate progress in obesity prevention'. The expert committee report explicitly recommends policy-makers to prohibit children's and adolescents' access to sugared drinks in schools, and that governments implement fiscal policies, including 'substantial and specific excise taxes' to reduce overconsumption of sugared soft drinks.
Mayor Bloomberg weighs in
At the end of May 2012, New York City Mayor Michael Bloomberg proposed a ban on the sale of supersized portions of sugar-sweetened drinks over 16 ounces (480 ml) in public venues (photo above at right). The proposed ban, part of a comprehensive strategy to improve the health of the more than 8 million New Yorkers (31), echoes several recommendations in the IOM report. The proposed portion size restriction would affect any business defined as a 'food service establishment' legally regulated by the NYC Department of Health. There are exemptions. The measure does not apply to drinks under 25 calories/8 ounce serving (240 ml), or to diet sodas, fruit juices, dairy-based drinks including milk-shakes, hot drinks such as coffee, or alcoholic drinks, or to drinks sold in grocery stores or convenience stores.
Within days of the Mayor's announcement, a food- and tobacco industry-financed front organisation paid for a full-page advertisement in The New York Times branding Bloomberg 'The Nanny'. It accused him of overstepping his authority and proposing a policy measure that infringed the right of individuals to choose whatever they want to purchase and consume. Attacks and satirical comments came from other quarters, together with many supportive responses. My thought was, as the elected highest official policy-maker responsible for protecting the health of his citizens, isn't Mayor Bloomberg simply doing his job?
In June 2012, last month as I write, the New York City Department of Health and Mental Hygiene posted a public hearing notice to gather feedback about the proposed measure, which has the overall intention of making smaller drink portions normal again, in areas where it has jurisdiction. The New York City Board of Health will ultimately approve or reject the proposal, taking into account the range of feedback received. This includes the decision of the American Medical Association to recommend a sugared drink tax as an effective way to finance consumer education campaigns and other obesity-related programmes (32).
As mentioned, in 2006 the City banned the use of trans-fats in foods and meals prepared by restaurants (15). New York was also the first US city to ban smoking in public places, including bars and restaurants. Another first was the 2003 support for calorie labelling disclosures in restaurants. This created the momentum for a federal law passed seven years later in 2010 to require calorie labelling in chain restaurants. Such measures make New York City legislators the pioneers in the US who have continuously re-defined what is possible and achievable to improve public health outcomes (33).

The City of New York City campaigns on supersized products and sugared soft drinks (above) have become increasingly powerful and direct over time
As you can see above, the New York City proposed ban on supersized portions of sugared drinks is the latest move in a carefully planned strategy to change the habits and culture of New Yorkers. The official campaigns are now sometimes almost as powerful as those now used to warn people against smoking. For example, the picture in the centre above shows a man with an amputated leg, an outcome of poorly managed type 2 diabetes, which research conducted by Association founder member Barry Popkin and colleagues show is linked to sugared soft drink over-consumption (34). In 2009 New York City initiated a Pouring on the Pounds counter-advertising campaign to encourage citizens to choose drinks with fewer calories, warning them not to 'drink themselves fat' (picture at left).This was followed by other campaigns that raise awareness of the consequences of excessive food portions (35) (middle photo) and a national campaign spearheaded by the CSPI (right) called 'Life's Sweeter with Fewer Sugary Drinks' (36).
In September 2013, Michael Bloomberg's terms come to an end, and New York City voters go to the polls. Will the next mayor maintain these public health initiatives? Perhaps, but probably without such boldness and flair. We will wait and see.
Conclusion
So having come to the end of my explorations so far, here are my reflections on what can be learned from these experiences.
Governments and other stakeholders have been working to improve the nutritional quality of food supplies for many decades. A priority since the 1980s has been to monitor, address, halt and reverse the co-epidemics of obesity, diabetes, cardiovascular disease, and other chronic non-communicable diseases. Policymakers are testing various approaches. Case studies are important to inform current and future efforts to increase the amounts of healthy foods and to decrease and amounts of unhealthy products, and in this way create habits, cultures and social norms where it is easy, normal, natural and affordable to choose a healthy diet.
Left to themselves, legislators will tend to prefer soft policy options, including collaboration with industry and other vested groups through voluntary multisectoral alliances or public-private partnerships. These can be productive when interests are shared or convergent.
To accelerate the pace of progress, national, state and city governments are now also experimenting with harder policy options usually involving legislation, such as regulation, taxation and bans. These approaches are often urged by public health and consumer advocacy organisations when soft policies and actions are perceived as inadequate. Both soft and hard approaches are natural experiments. Governments are responsible and accountable for ensuring that there are institutionalised and adequately funded mechanisms for independent monitoring and evaluating the outcomes of their policies.
Take trans-fats as an example. Progress in meeting the target of less than l per cent of calories per person per day has been accelerated in the countries that have combined voluntary approaches (industry partnerships and voluntary labelling disclosure) with regulatory or legal approaches (mandatory labelling disclosure or bans). Legislators have a great range of types and degrees of policy options. These include partnering with industry to encourage, recognise and reward positive changes to remove substances of concern. They also include the use of mandatory labelling to create a level playing field to influence industry-wide practices. They further include taxes on unhealthy products, which may well motivate industry to change faster, and can also raise revenue to support public health programmes.
I believe that governments need to hear from all stakeholders, including industry and its associates, public interest and citizen action organisations, scholars and researchers, and private foundations. President Barack Obama once said: 'Being deliberative, being inclusive, being thoughtful, doesn't mean everyone gets their way…It just means you get input from all sides'.
Surely what many of us who work in public health want, is to help to shape our societies so that healthy ways of life are normal and desirable, and everyone has options within the environments they live, work and play to eat healthfully and to be physically active. These changes can evolve when governments use a diverse and comprehensive policy tool-kit where timing, and the type of policies used, are a mix of art, skill, science and context. Governments have the legal authority to protect peoples' health. I believe that they must act to transform food supplies and reduce the growing burdens of overweight, obesity, and diet-related chronic non-communicable diseases (37).
References
- Pollan M. Unhappy meals. The New York Times, 28 January 2007.
- Willett WC, Stampfer MJ, Manson JE, Golditz G, Speizer F, Rosner B, Sampson L, Hennekens C. Intake of trans fatty acids and risk of coronary heart disease among women. Lancet. 1993; 341 (8845): 581-585. http://www.thelancet.com/journals/lancet/article/PII0140-6736(93)90350-P/abstract.
- Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. New Eng J Med. 2006; 354: 1601-1613. http://www.nejm.org/doi/pdf/10.1056/NEJMra054035.
- Abend L. Beating butter: Denmark imposes the world's first food tax. Time World. 6 October, 2011. http://www.time.com/time/world/article/0,8599,2096185,00.html.
- Bech-Larsen T, Aschemann-Witzel J. A macromarketing perspective on food safety regulation: The Danish ban on trans-fatty acids. J Macromarketing. 2012;32 (2):208-219. http://jmk.sagepub.com/content/early/2012/02/28/0276146711435262.
- Stender S, Dyerberg J. The influence of transfatty acids on health. Fourth edition. Danish Nutrition Council. 2003. http://www.meraadet.dk/gfx/ uploads/rapporter_pdf/Trans%20fatty%20acids_4.th%20ed._UK_www.pdf.
- Ministry of Food, Agriculture and Fisheries.Danish Veterinary and Food Administration.Trans fatty acid content in food. 27 February 2012. http://www.foedevarestyrelsen.dk/english/Food/Trans%20fatty%20acids/
Pages/default.aspx. - World Health Organization. Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in Human Nutrition, 10-14 November 2008. Geneva: WHO, 2008. http://www.who.int/nutrition/topics/FFA_summary_rec_ conclusion.pdf.
- Addy R. Danish Government considers abandoning fat, sugar tax. FoodNavigator.com. July 11, 2012. http://www.foodnavigator.com/content/view/print/654012.
- Jacobson MF. FDA is not protecting consumers from unsafe food additives. The Huffington Post. 11 July 2012. http://www.huffingtonpost.com/ michael-f-jacobson/food-additives-_b_1654034.html
- Brandt E. Trans-fatty acid levels in white adults. J Am Med Assoc. 2012; 307 (22):2870. Letter to the editor. http://jama.jamanetwork.com/article.aspx?articleid=1182850.
- Rahkovsky I, Martinez S, Kuchler F. New Food Choices Free of Trans Fats Better Align U.S. Diets With Health Recommendations. Economic Information Bulletin No.(EIB-95).Economic Research Services, United States Department of Agriculture. April 2012. http://www.ers.usda.gov/publications/eib95/.
- Dietz WH, Scanlon KS. Eliminating the use of partially hydrogenated oil in food production and preparation. JAMA. 2012; 308 (2):143-144. http://jama.jamanetwork.com/article.aspx?articleid=1216486.
- Center for Science in the Public Interest.Trans fat drop huge public health progress, says CSPI. 8 February 2012 [news release]. http://www.cspinet.org/new/201202081.html.
- Lueck TJ, Severson K. New York City bans most trans fats in restaurants. The New York Times, 6 December 2006. http://www.nytimes.com/2006/12/06/nyregion/06fat.html.
- Levine D. Judge sides with Cleveland in its transfat ban. Reuters. 12 June 2012. http://www.reuters.com/article/2012/06/13/us-usa-food-ohio-idUSBRE85C00H20120613.
- Branson C, Duffy B, Perry C, Wellings D. Acceptable Behaviour? Public opinion on behaviour change policy. Ipsos Mori Social Research UK, January 2012. http://www.ipsos-mori.com/DownloadPublication/1454_sri-ipsos-mori-acceptable-behaviour-january-2012.pdf
- Food Standards Australia and New Zealand.Roundtable on trans fats in the quick service restaurant industry – report on survey of progress of voluntary initiatives to reduce trans fatty acids in the Australian Food Industry Supply. July 2009. http://www.health.gov.au/internet/main/ publishing.nsf/Content/F5F93016C243672FCA2578A20019F090/$File/Trans-Fatty-Acids-in-the-Australia-and-New-Zealand-Food-Supply%20-%20Att3.pdf.
- Food Standards Australia and New Zealand. Review Report. Trans Fatty Acids in the New Zealand and Australian Food Supply. July 2009. http://www.foodstandards.gov.au/_srcfiles/TFAs _Aus_NZ_Food%20. Supply.pdf.
- Food Standards Australia and New Zealand.Trans fatty acids. December 2010. http://www.foodstandards.gov.au/consumerinformation/transfattyacids.cfm.
- Clarke R, Lewington S. Trans fatty acids and coronary heart disease. Food labels should list these as well as cholesterol and saturated fat. BMJ. 2006; 333(7561):214. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1523500/pdf/bmj33300214.pdf.
- National Institute for Health and Clinical Excellence. Prevention of cardiovascular disease at the population level. Public health guidance, PH25. London, UK, June 2010.http://www.nice.org.uk/nicemedia/live/13024/49273/49273.pdf.
- Department of Health. Public Health Responsibility Deal. Sign up and improve public health in England. 24 March 2012. http://responsibilitydeal.dh.gov.uk/category/food-network/. Artificial trans fat removal signatories: http://responsibilitydeal.dh.gov.uk/f3-artificial-trans-fat-removal/. 2012.
- Which? Government must do more to tackle the obesity crisis, says Which? The Government's Responsibility Deal is inadequate. 15 March 2012 [press release]. http://www.which.co.uk/news/2012/03/government-must-do-more-to-tackle-the-obesity-crisis-says-which-281403/
- Mytton OT, Clarke D, Rayner M. Taxing unhealthy food and drinks to improve health. BMJ. 2012; 344:1-7. http://www.bmj.com/content/344/bmj.e2931?view=long&pmid=22589522
- Rudd Report.Soft Drink Taxes: A Policy Brief.Yale Rudd Center, New Haven, CT. 2009..http://www.yaleruddcenter.org/resources/upload/docs/what/reports
/RuddReportSoftDrinkTaxFall2009.pdf./ - Nuffield Council on Bioethics.Public Health: Ethical Issues. UK: Cambridge Publishers, 2007. http://www.nuffieldbioethics.org/sites/default/files/Public%20health%20-%20ethical%20issues.pdf.
- Healthy Eating Research (HER).Sugar-Sweetened Beverage Taxes and Public Health. Research brief. HER and Bridging the Gap. July 2009.
http://www.healthyeatingresearch.org/images/stories/her_research_briefs/
ssb_taxes_and_public_health_herresearch_brief_7.31.09_final.pdf. - Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, Ludwig DS. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009; 361:1599-1605. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3140416/pdf/nihms308288.pdf.
- Glickman D, Parker L, Sim LJ, Del Valle Cook H, and Miller EA, eds; Committee on Accelerating Progress in Obesity Prevention; Food and Nutrition Board; Institute of Medicine.Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press, 2012. http://www.nap.edu/catalog.php?record_id=13275.
- New York City Task Force. Reversing the Epidemic: The New York City Obesity Task Force Plan to Prevent and Control Obesity. 31 May 2012. http://www.nyc.gov/html/om/pdf/2012/otf_report.pdf
- American Medical Association. AMA adopts policy addressing obesity, beverages with added sweeteners. 20 June 2012 [news release]. http://www.ama-assn.org/ama/pub/news/news/2012-06-20-ama-policy-addresses-obesity.page.
- Alcorn T. Redefining public health in New York City.The Lancet. 2012;379:2037-2038. .http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)60879-4/fulltext.
- Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356-1364.http://circ.ahajournals.org/cgi/reprint/121/11/1356.
- New York City Department of Health and Mental Hygiene.Health Department launches new ad campaign spotlighting increasing portion sizes and their devastating consequences. New York City posters encourage New Yorkers to cut their portions to reduce their risk of health problems. Press release. 9 January 2012. http://www.nyc.gov/html/doh/html/pr2012/pr001-12.shtml.
- Center for Science in the Public Interest. Cities, CSPI & health groups announce major new campaign to reduce soda consumption. 'Life's Sweeter with Fewer Sugary Drinks', says health officials [press release]. August 31, 2011.http://www.fewersugarydrinks.org/elements/pdf/LifesSweeter_LaunchRelease.pdf.
- Swinburn B. Obesity: Why governments must act. [Commentary]. World Nutrition July 2012, 3, 7, 307-325. Obtainable at www.wphna.org
Acknowledgement and request
Concept, drafting and final text approval: VK. Funding for this commentary: None. Conflicting or competing interests: None. The first complete draft was reviewed by Mark Lawrence and Boyd Swinburn of Deakin University's World Health Organization Collaborating Centre for Obesity Prevention in Australia, and by Mike Rayner and Oliver Mytton of the British Heart Foundation Public Health Research Group in the Department of Public Health at the University of Oxford in England. Geoffrey Cannon, Editor of World Nutrition, also made insightful contributions and comments.
Readers may make use of the material in this commentary if acknowledgement is given to the Association, and WN is cited. Please cite as: Kraak V. Food supplies. Trans-fats. Government policies and actions to protect citizen health. [Commentary].World Nutrition, August 2012, 3,8, 337-357. Obtainable at www.wphna.org.
All contributions to World Nutrition are the responsibility of their authors. They should not be taken to be the view or policy of the World Public Health Nutrition Association (the Association) or of any of its affiliated or associated bodies, unless this is explicitly stated.