World Nutrition
Volume 3, Number 7, July 2012
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary: Obesity
Why governments must act

Boyd Swinburn
Department of Population Nutrition and Global Health
University of Auckland, New Zealand
WHO Collaborating Centre for Obesity Prevention
Deakin University, Australia
Email: boyd.swinburn@auckland.ac.nz
Click here for member's profile
Introduction
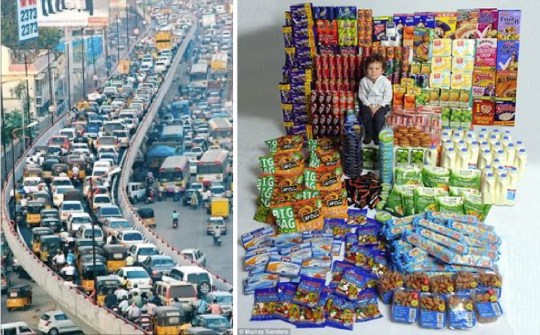
Traffic jam in Bangalore, India (at left); ultra-processed products and other energy-dense food consumed by British 4-10 year-olds in a year (at right)
The commercial drivers of the obesity epidemic are so influential that obesity can be considered a robust sign of commercial success – consumers are buying more food, more cars, and more energy-saving machines (1). It is unlikely that these powerful economic forces will change sufficiently in response to consumer desires to eat less and move more, or to corporate desires to be more socially responsible. When the 'free market' creates substantial population detriments and health inequalities, government policies are needed to change the ground-rules in favour of population benefits.
Concerted action is needed from governments in four broad areas (2). These are as follows. Governments should:
- Provide leadership to set the agenda and show the way
- Develop and implement policies (including laws and regulations) to create healthier food and activity environments
- Secure increased and continued funding to reduce obesogenic environments and promote healthy eating and physical activity
- Advocate for a multi-sector response and establish the mechanisms and support systems for all sectors to engage and enhance action
Policies, laws and regulations are often needed to drive the environmental and social changes that, eventually, will have a sustainable impact on reducing obesity. An 'obesity impact assessment' on legislation such as public liability, urban planning, transport, food safety, agriculture, and trade, may identify 'rules' which contribute to obesogenic environments which need to be modified to become healthier.
In other areas, such as marketing to children, school food, and taxes or levies, there may be opportunities for regulations that will actively support obesity prevention. Legislation in other areas, such as that designed to reduce climate change, improve urban liveability, and reduce traffic congestion, may also contribute to obesity prevention. (These are so-called 'stealth interventions' which have other primary aims, but as a consequence also reduce obesogenic environments and behaviours (3). A political willingness to use policy instruments to drive change will probably be an early hallmark of successful obesity prevention.
The obesity pandemic
Historically, with the exception of a few countries like the US, obesity prevalence rates have been low and relatively unchanging until about 20-30 years ago. In countries where regular monitoring of population heights and weights have been in place for several decades, a fairly consistent upward inflection was seen in the prevalence of obesity from about the early 1980s in children (4) and adults (5,6). Surveys from around the world now confirm that obesity has reached pandemic proportions, with many low-income countries now struggling under the double burden of continuing high rates of infectious diseases and undernutrition, and also now rising rates of obesity, diabetes and cardiovascular diseases (7).
No country has managed to reduce the burden of obesity using active public health approaches. The possible exception is Singapore with its Trim and Fit programme for children (8), although aspects of the programme have recently been revised because of the risk of stigmatising obese children by singling them out for extra exercise sessions.
The drivers are global and recent
The drivers of this pandemic, now affecting rich and poor countries alike, must be global in nature and relatively recent in onset. While biological hard-wiring explains the potential for the development of obesity, it cannot explain the secular trends in obesity prevalence. Humans have, for good survival reasons, evolved a biology that is designed to maximise energy intake and minimise physical activity. We seek and enjoy good tasting food, especially sweet, fatty and salty foods which tend to be ultra-processed and energy dense (9), and we seek to reduce the effort needed to do work by using machines and technology that do it for us.
While these are powerful factors, our biology has not changed over the last 30 years. What has changed dramatically is the environment around us – especially the easy availability of foods and energy-saving machines that feed those biological desires. It is the increasingly obesogenic environments which are promoting especially excessive energy intake but also reduced physical exertion, that are driving secular trends (10).
Environments that affect our behaviours can be broadly categorised into physical (what is or is not available), economic (the financial factors), policy (the 'rules'), and socio-cultural (the attitudes, beliefs, perceptions, values and norms of the societal or cultural group) (11). This has been a helpful and robust framework for scanning obesogenic environments and creating comprehensive lists of potential elements external to individuals that may influence behaviours. However, this list does not tell us which of these types of environmental factors are likely to be dominant as the drivers of the epidemic, or as the potential solutions that are urgently needed to turn the epidemic around.
The proposal in this commentary is that the dominant environmental drivers of obesity are economic, and that the dominant solutions will need to be policy-based. Before examining these two components in more detail, the other aspects of obesogenic environments are placed in the context as likely contributors to the epidemic.
The urban environment
The built urban environment has many physical features which influence physical activity levels: transport systems, recreation facilities and spaces, aesthetics, street design, land use, access to destinations like shops and schools, and so on (12). In many cities, these features are obesogenic although, being structural, they are usually quite slow to change and are therefore likely to be moderating or modulating factors rather than triggering factors for the recent rise in obesity prevalence. Moderators are those influences which either accentuate or attenuate the influence of the epidemic drivers on a population's prevalence of obesity (13). A much more rapid environmental change that promotes physical inactivity has been the flood of technology that provides increasing numbers of labour-saving devices and passive entertainment options.
The economic environment
However, the biggest obesogenic environmental change has been the increased availability and promotion of cheap energy-dense foods (14). There are some aspects of the policy environment (the 'rules') that may be inadvertently contributing to obesogenic environments. These include the increasing reach of public liability laws (for example, causing schools to lock their grounds after hours), farm policies in the US and Europe that subsidise fat and sugar production and keep fruit and vegetable prices high, and urban planning regulations that promote single rather than mixed land use in cities.
The socio-cultural environments that influence food, eating patterns, physical activity and body image vary enormously across populations. These influences undoubtedly explain many of the differences in obesity prevalence among populations and sub-populations (15,16). For example, cultures may differ in the expectations that they place on hosts (to over-provide food) and guests (to over-consume food), the appropriateness for girls and women to be physically active, the status of certain foods or dishes, the beliefs in the value of food and physical activity for health or the attitudes to large or slim body sizes (17).
This may mean that the socio-cultural differences between groups may confer a relative predisposition to or protection from weight gain when the group is exposed to a modern obesogenic environment. The variation of obesity prevalence, which has been from less than 1 per cent (India) to nearly 60 per cent (Tonga) (5), suggests that socio-cultural differences are very important. However, these are probably best thought of as moderating factors that either enhance or cushion the effects of the real drivers of the obesity epidemic. The concept of 'socio-cultural predisposition' to obesity is more akin to 'genetic predisposition' implying an underlying state which needs a change in context to become manifest. A leading US authority on obesity, George Bray, famously stated that 'genes load the gun, but the environment pulls the trigger' (18). This could now be updated to 'genes and culture load the gun, but the economic environment pulls the trigger'.
Market failure, commercial success
As mentioned, the two broad obesogenic changes in the environment that have noticeably increased in the past 30 years have been the upsurge in obesogenic food and in machines. Energy-dense foods and drinks are now readily available, highly promoted, and low-cost (19-21). There are two types of machines that reduce energy expenditure. These are labour-saving devices such as cars, computers, and occupational and domestic machines; and passive entertainment machines such as television, video, and electronic games (22,23).
The list of commercial products which promote excessive energy intake or decreased energy expenditure is very long, and those products are usually heavily marketed (cars and foods are the two highest advertised products (24). By comparison, the list of products that would maintain a healthy energy intake (like fruit and vegetables) or increased physical activity (like bicycles) is much shorter and their marketing budgets are tiny (1).
The driving forces behind the over-consumption of these obesogenic products are commercial (profit incentives). 'Market economies' remain the backbone of all leading economic systems. High consumption constitutes a 'commercial success' because the sellers make a profit, but to be considered a 'market success' both sellers and buyers need to gain from the transaction (25). The buyers, in the short term, certainly do gain. They get good tasting food at low prices, and lots of it if they eat at buffet restaurants or buy two-for-one, or up-size their serving to get better value for money. At a relatively low cost, they get enjoyable entertainment, new energy-saving domestic appliances to open tin cans or blow the leaves from their driveways, and more automatic features in their car. At one level, this is a 'market success' because customers are apparently making free choices to satisfy their needs and desires – or in economic jargon making 'preference decisions to maximise their utility'.
However, in the long term, people do not like to be obese – it is not their 'preference', nor does it give them high utility (in this case, good health and quality of life). Humans are notoriously prone to choose more for instant gratification than for long term benefits, and they are also prone to the marketing pressures which 'create' the desires in the first place (26). All these points particularly apply to children, who are much more dominated by short term desires than long term outcomes. Indeed, all the requirements of market failure are fulfilled by the marketing of unhealthy foods to children (13). Commercial drivers may also explain, in part, the increasing inequalities seen with obesity. People living in lower income areas often have less access to public transport and recreation facilities, and are more heavily targeted by fast food restaurants (27).
The increasing obesity prevalence and inequalities can, therefore, be described as a 'market failure'. This is because existing systems are failing to promote and sustain long-term individual and social goals (28). In orthodox economic theory, 'market failure' is an important signal for governments to intervene with policies and regulations that alter the market place so that the population can gain greater long-term utilities (29). Governments commonly enact policies which curtail commercial activities and individual choices in order to improve health outcomes such as reductions in the road toll, smoking, illicit drug use, workplace injuries, and so on. The case for government policy intervention in the commercial market place, to improve health and quality of life and reduce health inequalities by reducing obesity, is strong, particularly for children.
Government responses to date
In an ideal world, governments would have been monitoring population obesity trends, and would have acted early to implement the actions needed to halt and reverse the obesity epidemic. While this is eminently achievable given what we know today, it is not the common reality. Only a handful of countries even have monitoring systems in place to detect changes in the prevalence of obesity and its risk factors. For example, Australia has had only three national surveys of childhood obesity in 1985, 1995 and 2007 (29). For an epidemic that started a quarter of a century ago in such a rich country, and is probably now the single biggest threat to the health of Australian children, this is an incredibly poor performance.
It was only when the childhood obesity epidemic started featuring regularly in the media in the early 2000s (30) that governments and the public started to take notice. In response, many countries developed task forces and action plans which laid out the policies and programmes to promote healthy eating, physical activity and healthy weight. By and large, these plans could be described as comprehensive and evidence-informed, and probably would be effective if implemented.
However, almost universally, these plans have not been fully implemented, with typically only the peripheral, 'soft' components such as education and community programmes being supported. As an example, the Australian and New Zealand plans (31, 32), which are very good on paper, have failed to convert any of their core policies and regulations into action, rendering them weak and ineffective. Some examples of policy leadership have come from the New South Wales and Queensland governments, but the good start made by the New Zealand government to improve the healthiness of foods sold in schools (33-35) was thwarted by a change in government with the new minister for health reversing the healthy school food policy.
Roles for governments
We are now at a point where governments are belatedly aware of the threat that rising rates of obesity poses to population health, and also to economic well-being and the natural environment (36). The awareness of the size and complexity of the problem is also evolving into an awareness of the need for multiple actions to achieve a high enough 'dose of solutions'. There is widespread agreement that a multisectoral response will be needed from governments, the private sector, civil society and the public (37).
Within this societal approach, what are the roles of governments? Table 1 outlines the four broad roles for governments in the efforts to turn the obesity epidemic around. These are leadership, advocacy, funding, and policy. The table also provides the rationale to demonstrate how important the roles of government are, and some examples illustrate the concrete actions that can be taken. Government policy is fundamental as an early driver for change across society. This is the main focus of the remainder of this commentary.
Table 1
Roles of government in obesity prevention
Leadership
Description
Providing a visible lead
Reinforcing the seriousness of the problem
Demonstrating a readiness to take serious action
Rationale
All societal change needs strong leadership
The role of governments is central and powerful
Governments have enough authority to stimulate a sustained multi-sector response
Government voices speak loudly about problems
Government actions speak louder about solutions
Examples
Being visible in the media
Role modelling healthy behaviours (at personal, community levels)
Role modelling healthy environments (at government agency level)
Creating mechanisms for a whole-of-government response
Lifting the priority for health (versus commercial) outcome
Policy
Description
Developing, implementing, and monitoring a set of policies, regulations, taxes, and
subsidies that make environments less obesogenic and more health promoting
Rationale
Impact of environmental factors (physical, economic, policy, socio-cultural)
Changing environments often requires policy drivers
Education-based approaches are weak without supportive environments
Examples
Banning the marketing of unhealthy foods to children
Subsidising public transport and active transport more than car transport
Requiring 'traffic light' front of pack labelling of food nutrient profiles
Restricting the sale of unhealthy foods in schools
Funding
Description
Securing increased and continuing funding to create
healthy environments and encourage healthy eating and physical activity
Rationale
Changing environments requires funding
Social marketing and programmes require funding
Supporting actions (such as training, research, evaluation, monitoring) require funding
Public good funding comes mainly from government sources
Examples
Establishing a health promotion foundation to fund programmes and research
(Funding could come from a hypotheticated tobacco tax)
Moving from project funding to programme and service funding for obesity prevention
Creating centres of excellence for research, evaluation and monitoring
Advocacy
Description
Advocating for a multi-sector response across all societal sectors (governments, the private sector, civil society, and the public)
Rationale
Solutions need to involve many sectors within governments,all sectors outside government
Authoritative mechanisms needed to achieve cross-sectoral collaboration, coordination
Examples
Advocating to the private sector for corporate responsibility on marketing to children
Creating a high-level taskforce to oversee and monitor multi-sector actions
Encouraging healthy ways of life for individuals, families, communities
The policy backbone
As identified by WHO in the Global Strategy on Diet, Physical Activity and Health (37), the impetus for change needs a critical level of political leadership and some defined policy directions to address obesity. The policy instruments include the 'softer' approaches of social marketing, health promotion programmes, and government advocacy for changes in individual and organisational behaviour, as well as the 'hard' policies of laws, regulations, enforceable policies, and fiscal instruments (38). The softer instruments are preferred by most governments, but there are growing calls for the law to be used to help tackle obesity (39).
It is entirely possible that 'softer' interventions, such as health education, may increase health inequalities if it they are picked up more by higher-income people than lower-income people. Laws and regulations, on the other hand, tend to be applied across the board, so state policies banning vending machines in schools should at least not increase inequalities and in fact may reduce them if the schools in poorer areas had more vending machines in the first place.
If the harder end of policy is to be applied, what would a substantive, effective 'policy backbone' for reducing obesity look like? Clearly, a comprehensive set of policies would cover the possibilities for action at all levels of government. Examples of analysis grids for policies which may influence obesity have been developed (40, 41). It is clear that there are many policy barriers to healthy eating and physical activity and many gaps that health-promoting policies could fill.
Importantly, virtually all of the hard policy options are directed at the environment (making the healthy choice the easy choice) and virtually all of the policies that directly target people are softer options (encouraging people to make the healthy choice). This gives the lie to the perception, emphasised by some private sector interests, that government policies will result in a 'nanny state' – implying that the state will be telling people what they can and cannot eat. Governments have not shied away from requiring certain behaviours of their citizens when the public health threat is high. Seatbelts, workplace safety, smoke-free areas, and controls on illicit drugs are common, everyday examples. But requiring certain eating and physical activity behaviours to prevent obesity or chronic diseases is highly unlikely to happen.
Some of the policy options will be making existing laws and regulations less obesogenic. For example, an unintended consequence of regulations prohibiting the importation of fruit such as bananas and apples into Australia may mean that consumers pay more (and thus presumably eat less) of these foods. Conversely, subsidies on sugar and plant oil production will make energy-dense foods cheaper (and thus stimulate consumption). People's consumption patterns are very price dependent (42, 43). An 'obesity impact assessment' may be a form of health impact assessment that needs to be applied to such policies at the time of their formulation.
Many government policy options have significant commercial implications It is not surprising that some of these proposals, such as banning junk food marketing to children (44), encounter heavy opposition from the corporate sector. This opposition, currently being led by the food and advertising sector, but which will no doubt be joined by the automobile and oil companies in the future, is one of the major hurdles that governments face in making regulations for obesity prevention. 'Reducing red tape' has been a strong policy direction from many governments for some years, so making more regulations will also run counter to this philosophy. For some policy interventions, such as the universal measurement of body mass index (BMI) in children and sending a 'BMI Report Card' back to parents (45), there may be public opposition to contend with as well.
Lessons from other epidemics
Tackling many other public health epidemics and threats in the past has required a backbone of hard policies around which the softer options can work to amplify their effectiveness (46,47). Tobacco control is the classic case: taxation, advertising bans, and smoke-free environments legislation, served as the drivers for change with quit programmes, social marketing and education providing added value (48,49).
Reducing the road toll of deaths and injuries has required a substantial number of laws and regulations around speed, seat belts, vehicle safety, drink driving and so on, to which has been added social marketing and education campaigns and a large amount of vehicle safety enhancements (50).
Infectious disease control is a highly regulated public health endeavour, as is the control of poisons and toxins. Reductions in cardiovascular diseases have been dominated by medical interventions (51) which have proved to be an effective, albeit very expensive approach. Legal and policy interventions are available to reduce cardiovascular diseases (52), but they tend to remain in the realm of 'could do' rather than 'have done' options.
Many parallels have been drawn between other epidemics and the obesity epidemic. Tobacco control is the usual analogy (53). This is rebutted by the food industry with the statement that food and tobacco are completely different. This is true, but the observed patterns of corporate responses to the public health pressure for regulations, and the required spectrum of solutions for the epidemics, including regulatory and fiscal interventions, are remarkably similar.
Even though legislation for obesity prevention could not be directly aimed at eating and physical activity behaviours, any 'rule-based' approach (even at the level of school or home rules) is likely to be a powerful way of changing social norms and attitudes. For example, a policy banning high fat or sugar foods and drinks from school canteens can be expected to accelerate the transition in norms from canteens full of products high in fat, sugar and salt, to canteens with foods that match those promoted in the school's nutrition curriculum. In countries like Australia where children mainly bring their school lunches from home, only a few percent of children's total yearly energy intake comes from the school canteen. However, having visible icons of healthy food are likely to be very important in influencing eating patterns outside school (54). Such policy interventions could be considered 'lighthouse' interventions: they cast their light far and wide and show children and parents the way forward for healthy eating.
Combined policies
Obesity is currently attracting public and political attention, but this may not be a lasting phenomenon. Indeed, the sloth and gluttony stigma associated with being obese means that the public pressure from obese people agitating for change is virtually non-existent. There is not a groundswell of overweight and obese people calling for action. The pressure is predominantly coming from the professional sector. Therefore, it will be important for obesity prevention advocacy to combine with other like-minded 'movements' to get policy action. Interventions which promote healthy eating or physical activity but are enacted for other reasons could be considered 'stealth interventions' (55). Three such 'movements' centre around climate change (56), congestion in cities (57); and the New Nutrition Science (58,59), which seeks to incorporate environmental outcomes, such as sustainability and minimising degradation, into the debate and science around nutrition and food systems.
Policies to reduce greenhouse emissions, such as corporate and individual carbon trading, would be powerful stealth interventions for obesity prevention (56). Congestion taxes (57), car-free cities (60), public transport growth (63), and other urban planning options (12), will increased physical activity as a beneficial side effect and thus contribute to obesity prevention. Reducing the carbon cost of food could also have an effect on energy intake since many of the energy-dense foods which promote obesity tend to be more processed, packaged foods – in other words, higher in carbon costs.
Conclusion
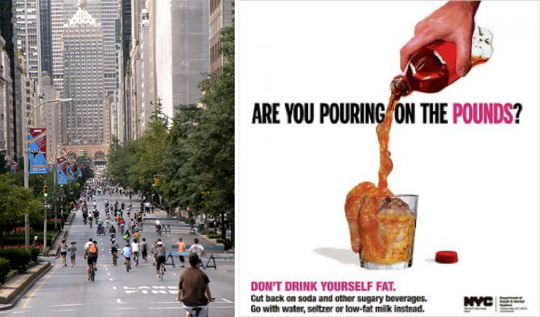
New York: a car-free morning in the City (left) and (right) City Hall's
campaign against sweetened soft drinks – by order of Mayor Bloomberg
Government policy leadership will be needed to accelerate effective action to reduce obesity and its associated inequalities. The suite of interventions will have to include some 'hard paternalism' policy options such as legislation and regulation, to make human environments less obesogenic. The calls for action from public health and community advocates in many countries are strong, especially around childhood obesity.
There are already some although as yet uncommon examples of real political leadership being added to the mix and, in those circumstances, real progress can be made. New York City Mayor Michael Bloomberg is currently the leading political figure in creating policy change for obesity prevention (62,63). In most places, however, the foremost challenge is to achieve that political leadership. All of the usual processes of political advocacy will be needed in this endeavour. But there is also substantial overlap between the solutions for obesity and the solutions for environmental sustainability, reduced congestion, and urban liveability. Collaborations across these movements will create greater pressure for change and greater coordination of action. Indeed for obesity, it may be that the 'stealth interventions' for environmental sustainability prove to be particularly powerful forces for checking and reducing rates of obesity
References
- Moodie R, Swinburn B, Richardson J, Somaini B: Childhood obesity - a sign of commercial success but market failure. Int J Ped Obesity 2006, 1 (3): 133-138.
- Sacks G, Swinburn B, Lawrence M. Obesity Policy Action framework and analysis grids for a comprehensive policy approach to reducing obesity. Obes Rev 2009; 10 (1):76-86.
- Robinson TN. Save the world, prevent obesity: Piggybacking on existing social and ideological movements. Obesity 2010; 18(suppl 1):S17-S22,
- Lobstein T, Frelut ML. Prevalence of overweight among children in Europe. Obes Rev 2003, 4(4): 195-200.
- International Obesity Taskforce: International Obesity Task Force Prevalence Data. http://www.iotf.org/database/index.asp.
- Finucane MM, Stevens GA, Cowan MJ, et al. National, regional,and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 2011; 377: 557–567.
- World Health Organisation. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva: WHO, 2000:
- Toh CM, Cutter J, Chew SK: School based intervention has reduced obesity in Singapore. BMJ 2002, 324, 427.
- Monteiro CA. Nutrition and health. The issue is not food, nor nutrients, so much as processing (Invited commentary). Public Health Nutrition. 2009; 12(5): 729-731.
- Egger G, Swinburn B: An 'ecological' approach to the obesity pandemic. BMJ 1997, 315 (7106): 477-480.
- Swinburn B, Egger G, Raza F: Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med 1999, 29 (6 Pt 1): 563-570
- Handy SL, Boarnet MG, Ewing R, Killingsworth RE. How the built environment affects physical activity: views from urban planning. Am J Prev Med 2002, 23 (2 Suppl):64-73.
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker S. The global obesity pandemic: shaped by global drivers and local environments. The Lancet 2011; 378: 804-814.
- Drewnowski A: Nutrition transition and global dietary trends. Nutrition 2000, 16(7-8): 486-487.
- Crawford PB, Story M, Wang MC, Ritchie LD, Sabry ZI: Ethnic issues in the epidemiology of childhood obesity. PediatrClin North Am 2001, 48(4): 855-878.
- Gordon-Larsen P, Adair LS, Popkin BM: The relationship of ethnicity, socioeconomic Factors, and overweight in US adolescents. Obes Res 2003, 11 (1): 121-129.
- McCabe MP, Mavoa H, Ricciardelli LA, Schultz JT, Waqa G, Fotu KF. Socio-cultural agents and their impact on body image and body change strategies among adolescents in Fiji, Tonga, Tongans in New Zealand and Australia. Obesity Reviews 2011, 12 (Suppl. 2), 61–67.
- Bray GA. Leptin and leptinomania. Lancet 1996, 348: 140-141.
- Drewnowski A, Popkin BM: The nutrition transition: new trends in the global diet. Nutrition Reviews 1997, 55(2):31-43.
- Cutler DM, Glaeser EL, Shapiro JM. Why have Americans become more obese? J Econ Perspect 2003; 17: 93–118
- Chou SY, Grossman M, Saffer H: An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ 2004, 23 (3):565-587.
- Lanningham-Foster L, Nysse LJ, Levine JA: Labor saved, calories lost: the energetic impact of domestic labor-saving devices. Obes Res 2003, 11 (10): 1178-1181.
- Vandewater EA, Shim MS, Caplovitz AG: Linking obesity and activity level with children's television and video game use. J Adolesc 2004, 27(1): 71-85.
- Advertising Age's special report: profiles supplement. 50th annual 100 leading national advertisers. Advertising Age; 2005.
- Bator F: The anatomy of market failure. Quarterly Journal of Economics 1958, 72: 351-379.
- Rice T. The economics of health reconsidered. 2nd edition. Chicago , Health Administration Press, 2002.
- Reidpath DD, Burns C, Garrard J, Mahoney M, Townsend M: An ecological study of the relationship between social and environmental determinants of obesity. Health & Place 2002, 8(2): 141-145.
- McCarthy M: The economics of obesity. Lancet 2004, 364(9452): 2169-2170.
- Gill TP, Baur LA, Bauman AE, et al. Childhood obesity in Australia remains a widespread health concern that warrants population-wide prevention programs. Med J Aust 2009; 190: 146-148
- International Food Information Council: Trends in obesity related media coverage.[http://www.ific.org/research/obesitytrends.cfm] .
- National Obesity Taskforce: Healthy Weight 2008 - Australia's Future - The National Action Agenda for Children and Young People and their Families. Canberra: Department of Health and Ageing; 2003.
- Ministry of Health New Zealand: Healthy Eating - Healthy Action, Oranga Pumau - Oranga Kai. Wellington, New Zealand , Ministry of Health; 2002.
- NSW Health: Fresh Tastes at School.[http://www.health.nsw.gov.au/obesity/adult/canteens.html]
- New Zealand Ministry of Health: Healthy Eating Healthy Action Food and Beverage Classification System. [http://www.moh.govt.nz/moh.nsf/indexmh/heha-foodclassification]
- Queensland Government: Healthy food and drink supply strategy for Queensland Schools. [http://education.qld.gov.au/schools/healthy/food-drink-strategy.html]
- Lang T, Barling D, Caraher M: Food, social policy and the environment: towards a new model. Social Policy and Administration 2001, 35( 5): 538-558.
- World Health Organization.: Global strategy on diet, physical activity, and health. [http://www.who.int/dietphysicalactivity/goals/en]
- Milio N. Nutrition and health: patterns and policy perspectives in food-rich countries. SocSci Med 1989, 29(3):413-423'
- Gostin LO. Public health law in a new century. Part I: law as a tool to advance the community's health. JAMA 2000, 283 (21): 2837-2841.
- Sacks G, Swinburn BA, Lawrence M: A systematic policy approach to changing the food and physical activity environments to prevent obesity. Aust N Z J Health Policy 5:13.
- Sacks G, Swinburn B, Lawrence M. Obesity Policy Action framework and analysis grids for a comprehensive policy approach to reducing obesity. Obes Rev 2009; 10 (1):76-86.
- Turrell G: Structural, material and economic influences on the food-purchasing choices of socioeconomic groups. Aust N Z J Public Health 1996, 20 (6): 611-617.
- French SA: Pricing effects on food choices. J Nutr 2003, 133(3):841S-843S.
- Hawkes C: Marketing food to children: the global regulatory environment. Geneva: World Health Organisation, 2004.
- University of Arkansas for Medical Sciences: Year Three Evaluation: Arkansas Act 1220 of 2003 to Combat Childhood Obesity. Little Rock, Arkansas , Fay W. Boozman College of Public Health,; 2006:34.
- Anonymous: Changes in the public health system. Morbidity and Mortality Weekly Report 1999, 48(50): 1-7.
- Swinburn B: Sustaining dietary changes for preventing obesity and diabetes: lessons learned from the successes of other epidemic control programs. Asia Pac J Clin Nutr 2002, 11 Suppl 3:S598-606.
- Mercer SL, Green LW, Rosenthal AC, Husten CG, Khan LK, Dietz WH: Possible lessons from the tobacco experience for obesity control. American Journal of Clinical Nutrition 2003, 77(Suppl): 1073S-1082S.
- Fichtenberg CM, Glantz SA, Association of the California Tobacco Control Program with declines in cigarette consumption and mortality from heart disease. N Engl J Med 2000, 343(24):1772-1777.
- Haddon W Jr.: Advances in the epidemiology of injuries as a basis for public policy. Public Health Rep 1980, 95(5): 411-421.
- Hunink MGM, Goldman L, Tosteson ANA, Mittleman MA, Goldman PA, Williams LW, Tsevat J, Weinstein MC: The recent decline in mortality from coronary heart disease, 1980-1990: the effect of secular trends in risk factors and treatment. JAMA 1997, 277(7 (Feb 19)): 535-542.
- Perdue WC, Mensah GA, Goodman MD, Moulton AD: A legal framework for preventing cardiovascular diseases. Am J Prev Med 2005, 29 (5S1): 139-145.
- Chopra M, Darnton-Hill I: Tobacco and obesity epidemics: not so different after all? BMJ 2004, 328(7455):1558-1560.
- Bell AC, Swinburn B: School canteens: using ripples to create a wave of healthy eating. MJA 2005, 183(1): 5-6.
- Robinson TN, Sirard JR: Preventing childhood obesity: a solution-oriented research paradigm. Am J Prev Med 2005, 28(2 Suppl 2): 194-201.
- Egger G: Personal carbon trading: a potential 'stealth intervention' for obesity reduction? Med J Aust 2007, 187:185-187.
- Roberts I: Congestion charging and the walking classes. BMJ 2003, 326:345-346.
- Cannon G, Leitzmann C. The new nutrition science. Public Health Nutr 2005; 8(6A): 673-694.
- The Giessen Declaration Public Health Nutr 2005, 8(6A):783-786.
- Crawford JH: Carfree Cities. Utrecht: International Books, 2000.
- Pikora T, Miller M: Promoting Active Transport - An intervention portfolio to increase physical activity as a means of transport. Melbourne: National Public Health Partnership, 2001.
- Mullin S, Marukutla N. Hard-hitting messages that work: NYC's public health education campaigns. Huffington Post, 7 February 2012.
- Schoen D. Bloomberg Big-Soda Ban: A Nuanced Plan That's Healthy For NYC. Forbes, 31 May 2012
Acknowledgement and request
Readers are invited please to respond. Please use the response facility below. Readers may make use of the material in this commentary, provided acknowledgement is given to the authors and the Association, and WN is cited. Please cite as: Swinburn B. Obesity: Why governments must act [Commentary]. World Nutrition, July 2012, 3, 7, 307-325.Obtainable at www.wphna.org. Please also state that it is an updated version of the paper in Australia and New Zealand Health Policy 2008, 5:12 doi:10.1186/1743-8462-5-12. Obtainable at: http://www.anzhealthpolicy.com/content/5/1/12
The opinions expressed in all contributions to the website of the World Public Health Nutrition Association (the Association) including its journal World Nutrition, are those of their authors. They should not be taken to be the view or policy of the Association, or of any of its affiliated or associated bodies, unless this is explicitly stated.