World Nutrition
Volume 3, Number 4, April 2012
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary. Public health and nutrition
Our vision: where do we go?

Geof Rayner, Centre for Food Policy, City University, London UK
geof@rayner.uk.com
Tim Lang, Centre for Food Policy, City University, London, UK
t.lang@city.ac.uk
Access pdf of this commentary here
Access pdf of associated short communications here
In this commentary we state that properly understood, public health nutrition is a crucial and central part of public health, which now must gain a leading role in the public health movement, with all this implies.
The first definition of 'public health' to command general support was made in 1920 by the US biologist Charles-Edward Winslow (1877-1957). This begins 'Public health is the Science and Art of preventing disease, prolonging life, and promoting health and efficiency' (1). It is a statement of aspiration – note 'Art' – and mostly a specification of tasks. We offer a new orientation, for the world we live in now:
'In this 21st century, the pursuit of public health requires analysis of the interactions between the material, biological, social and cultural dimensions of existence. This demands a new mix of interventions and actions to alter and ameliorate the determinants of health; the better framing of public and private choices to achieve sustainable planetary, economic, societal and human health; and the active participation of movements to that end. Ecological public health is about shaping the conditions for good health for all'.
Box 1
Editor's note
We are delighted to be publishing this powerful commentary in the month of our Rio2012 conference. Its conceptual framework, ideas, warnings and recommendations are in harmony with the general principles that have informed Rio2012.
Public health nutrition is part of public health. We have our own speciality and expert knowledge, but our wider purpose is to play our part to preserve, protect and enhance the conditions of life of society as a whole. The task is wider yet, because our duty also is to take into account the impact of our knowledge, policies and actions on the whole living and physical world and the biosphere.
Geof Rayner and Tim Lang have dedicated much of their professional lives to understanding what public health means now, in this now our new world. In their book Ecological Public Health, published by Routledge/Earthscan this month, they draw on the grand lessons learned in the golden 19th century era of public health knowledge, policy and action, which began to make European and North American cities safe and pleasant, protected wildernesses, forests and parks, and promoted equity. At that time, leading thinkers, reformers, scientists, politicians and industrialists debated – sometimes passionately – on the great issues of population health and well-being. They came to agree that nutrition is crucial and central to health; and that the general conditions of life, including health, are basic determinants of the adequacy and quality of nutrition.
They say that we now need to learn these lessons all over again. The great debates in Europe and then North America in the 18th and 19th century involved all types of leader, including novelists, poets, pamphleteers and agitators, as well as scientists, philanthropists, industrialists and politicians. These debates were about issues like increase in population, rapid increase of urban population, the capacity of agriculture and manufacture, the state of impoverished people, decent standards of work and life, and the ability of leaders of society to grasp and master crises.
Geof Rayner and Tim Lang say that that the issues that confronted industrializing Europe in the 18th and 19th centuries are rampant now on a global scale, and that what was achieved then, needs to be achieved now, including in our own work. We also need to have a good understanding of all relevant modern knowledge and insights. Their commentary develops the thesis of their book, with special attention to nutrition as part of public health. Tim is the first professor of food policy ever appointed, so there is plenty in the book and in this commentary about international food and nutrition knowledge, policy, and action.
Introduction
Public health nutrition is a central part of public health. It now faces huge challenges. As examples:
- The nutrition transition
The restructuring of food systems and supplies, and so dietary patterns, with rises in incomes, driving increased obesity and associated diseases worldwide. - Food insecurity
The increase of hunger, after decades of improvement. - Distorted food markets
Not just distortions from subsidies, but also distortion of human needs by the marketing of powerful corporate interests. - Environmental impacts
Not just climate change, but a web of threats, to water, land use, forest cover, soil fertility, and biodiversity. - Insecure employment
The majority of the world lives by farming, now threatened by international supply chains and the power of oligopolistic commodity markets. - Energy reliance
Food systems are based on petroleum, a fossil resource which is increasing in cost and on which farming, and therefore nutrition, depends.
So far, responses to these series of crises have mostly restated the claim that all will get better as more is produced. Like many others, we cannot agree. Here are five reasons why. First, there are gross inequalities of access and power which magnify the ill-effects of unhealthy food systems on incidence of serious diseases (2). Second, there is already a surplus of food energy (calories) in the world. Third, transnational and other vast food and drink corporations are penetrating lower-income countries with their fatty, sugary or salty ready-to-eat or to-heat energy-dense ultra-processed products – as shown by Carlos Monteiro and his colleagues in this journal (3). Fourth, food is being diverted to energy for biofuels, particularly in North and South America and Europe (4). Fifth, this analysis downplays the serious complications and crises for world and national food systems and supplies caused by environmental change and biodiversity stress (5).
The crises that we face
The net result is gross mismatch between food systems, natural ecology, commercial practice and public governance, and the state of public health. It would be unwise for nutrition scientists to ignore this mismatch or merely hope that it disappears. The problem overall is shown in Table 1, below.
Table 1
Impacts of food systems on sustainability
Modern agriculture currently contributes around 14 per cent of greenhouse gas emissions (6).
Of these, animals are responsible for 31 per cent, and fertilisers for 38 per cent (7).
In Europe, meat and dairy products account for 24 per cent of their environmental impact (8).
Approximately half of all cereals grown globally are fed to animals (9).
Of 24 of the world's ecosystem services, five are being degraded or used unsustainably. Food is a major source of this degradation (10).
Global agriculture consumes 70 per cent of all freshwater extracted for human use (11).
Intensive livestock production is probably the largest sector-specific source of water pollution (6).
It takes 200 litres of water to produce a 200 millilitre glass of milk, and 2400 litres of water to produce a 150 gram hamburger (12).
In the 20th century, about 75 per cent of the genetic diversity of domestic agricultural crops was lost (13).
Over half (52 per cent) of global wild fish stocks are 'fully exploited' (14).
More production is not the answer
For these and more reasons, we question any policy that once again asserts the priority of raising food production above all others. Production for what? Of what? For whom? At what cost? An emphasis on more production may well be required in the future. But it is now being used as a rationale by some scientists and policy-makers to sideline the case for systematic change, despite the ample evidence of serious public health harm from distorted food systems and supplies, and thus dietary patterns.
The dominant food and health policy narrative compounds this over-narrow thinking. It tantalises policy-makers with the proposition that the answer to almost any threat to food system capacity is technological innovation, usually involving increased exploitation of natural resources. But as in the mid 20th century, the rational and lasting solution is to reframe food systems. This requires an equal policy and scientific emphasis on supply, distribution, and consumption. This means a whole new relationship of humans to food, and to nutrition.
What looks like a long term perspective – matching food availability to population growth – provides only a crude and partial answer to food sustainability. It leaves out the critical public health dimension of sustainable food systems, and ignores the powerful evidence of environmental damage from intensive, monoculture farming and ever-longer food supply chains (5).
Dietary patterns have always been changing. But now, part of the public health crisis is due to the pace and scale of that change. Two examples are the vast increase in production and thus consumption of sugared soft drinks and of sugary energy-dense ultra-processed products, and the distortion of customer and consumer demand that is driven by commercial marketing power.
'Healthy lifestyle choices' are not the answer
The overwhelming evidence that public health continues to be damaged by pathogenic food systems has been resisted for decades. Now, policy-makers are beginning to accept that there are connections. But in proposing 'new diets', they still emphasise 'healthy lifestyle adjustment choices' and thus put the blame and responsibility on to consumers for making foolish choices. Part of this 'smoke-and-mirrors' policy miasma, are the emerging 'corporate responsibility' commitments. These are given by transnational food and drink corporations to national governments (and relevant UN agencies), for example, by way of agents such as the World Economic Forum (15), and the 'public-private partnership', the Gates Foundation-funded Global Alliance for Improved Nutrition (GAIN) (16).
Promotion of healthy diets is proposed almost entirely at individual level, and this despite the fact that in most parts of the world, people see themselves as members of families and communities – and quite right too. Attempts to stimulate collective change, even through the relatively easy 'soft' measure of food labelling, is bitterly contested. But at least the case for shifting dietary patterns with public health in mind is on the policy table. However, the case for shaping food supplies around eco-systems that are genuinely sustainable, and as such essential for planetary survival, has barely begun. The 2007-2008 oil price rises sent a shock through world agriculture, and have shaken even rich countries – whose governments prefer to see hunger as the key problem, safely located in impoverished countries. But the policy frameworks remain centred on pushing production, not on changing food systems in order to protect and improve public health.
Nutrition is political
What are public health nutrition professionals going to do about all of this? Some say that these 'political' issues should be kept out of nutrition, which should be 'neutral'. Others – including ourselves – state that nutrition professionals need now to rebuild and reconnect with their long, distinguished and effective tradition of engaging with wide social issues.
Nutrition seen with public health in mind is a social, cultural as well as a biological science. It needs to engage with the realities that shape people's daily lives. It needs to engage with the social, political and economic drivers of health and disease (17). The challenge for 21st century nutrition cannot be extricated from the other public health crises.
In this commentary we outline how public health, itself a mixture of traditions and perspectives, has been – and is and must be – engaged with fundamental ideas of the good society, in any present time and for future generations. We point out that the great 'classic' issues of public health that involve nutrition, such as rapid population growth, very rapid growth of cities and slums, grossly inadequate sanitary services, exploitation and even virtual enslavement of workers, food insecurity, hunger and starvation, and general immiseration, remain crises but now on a vaster scale. As well as these, explosive increases in obesity and chronic disease, most of all among impoverished populations, now amount to a new public health crisis. We also propose how public health nutrition can find its way in this world, as a vital contributor to genuine social, economic and environmental protection and development. We ask and try to respond to questions like these:
- How does nutrition fit within public health?
- What are the lessons from the past?
- What is the meaning of public health?
- What shapes the world that includes public health nutrition?
- Whither public health nutrition in this century?
The models of nutrition science
In this period now, the place of nutrition within public health is weak and confused, although it has been, and always should be, central and crucial. The fact to face is that public health nutrition these days, like clinical nutrition of which it is not a branch, has largely become reduced to a technical craft. Is that what public health professionals want, to be mainly or even only technicians? If yes, the whole profession becomes – or remains – a bit-player that occasionally enters the stage, laments, and exits, in a colossal epic drama enacted by social, economic and political forces not aligned with health improvement.
We have been engaged in public health for many years now, and we reject this assumption. We see public health nutrition as crucial in the shaping and invigoration of public health in this century – and the next.
Why has nutrition, and public health nutrition, become weak? Partly this is because nutrition is torn between at least three ways of thinking (18).
Biochemical
The dominant convention sees nutrition as a life science, essentially about analysing minute interactions down the explanatory scale, as a biochemical and physiological discipline, now also engaged with genetics. This quasi-medical model makes nutrition – often termed 'clinical nutrition' – personal only.
Social
In the second convention, nutrition is seen as the outcome and expression of societal forces such as class, income, status. In this model, the nutritional status of populations is largely determined by social forces.
Ecological
The third convention is ecological nutrition. This is an old convention which is now returning, driven by recognition of environmental pressures, and the need for nutrition once more to engage with planetary capacities to feed humans. This sees human nutrition as shaped by prior eco-systems, with nutritional health and culture existing within environmental limits, while also being embodiments of our ecological past.
YThese split approaches are part of the reason why nutrition is usually relegated to the margins of public policy. It doesn't use one language or speak with one voice.
But in the past, nutrition was a strong force for public health. In the 19th century, European nutrition scientists were at the centre of public policy planning and action, as they were in the early and mid 20th century (19). Even before the modern public health movement was first created and aroused, in the industrialising Britain of the 1840s, nutrition was at the heart of arguments about health and social progress. It was well understood that food and nutrition shapes life and health.
How we got to where we are now

Population growth and food and nutrition security: a big 18th century issue, for Adam Smith (left), Thomas Malthus (right). A bigger issue now (centre)
Serious discussion of nutrition is now usually presented as needing to be 'scientific'. But in the past it went far beyond what is now seen as science, at least in its biological dimension, and was typically engaged with social and political issues. Furthermore, many of the most influential thinkers in Europe, whose interests ranged far wider than what is now usually seen as the area of nutrition, were very well aware that the state of nations depended on secure, adequate, nourishing food supplies.
The issue of population
In the late 18th century Adam Smith (1723-1790), the philosopher, economist and key thinker in the Scottish Enlightenment, saw what is now known as nutrition as crucial to progress. He is now celebrated by right-wing ideologues as the architect of so-called 'free market' thinking, policies and practices. But this was not his actual position; he advocated good government working within moral frameworks.
In The Wealth of Nations (1776), he proposed that prosperity, or rise in the standard of living, was revealed not through ownership or money but through a society's rate of population growth (20). He reasoned that rapid population increase indicated abundant agricultural production (then the basis of wealth), and easy availability of food. This fed back into improving patterns of health, for which population growth was the leading indicator. Smith's key example was the British colonies of North America, with their abundant virgin farmland. Anthropometic studies have since proved him right; colonists were taller and healthier than even European aristocrats.
The English economist and demographer Thomas Malthus, who also was an ordained priest (1766-1834), took another view. In his 1798 Essay on Population (21), he countered the radical proposition, formed in the cauldron of the French Revolution, that political change alone was the key to social progress. He argued that even if a population was growing rapidly, the benefits might be episodic or short-lived. Population health depended on the consistently improving productivity of agriculture. If the growth rate of the former outran the latter, which he foresaw as likely, the result would be famine and disease.
For Thomas Malthus, human existence relied upon a delicate, often perilous, balance between population and agricultural output. He also thought there were interceding factors. Education had a role, for it could delay marriage and thus reduce fertility. Free trade too was a factor, although he had his doubts. Tariff-free trade – fiercely argued over in Britain at the time – boosted food availability but might make the country more reliant on foreign imports, thus undermining home producers. The long term outcome might be worse.
General political, economic and social theories
Debates and questions such as these, in which food and nutrition as then understood were central, led to the development of four of the most powerful general theories to shape modern society: capitalism, socialism, evolutionary theory (often called Darwinism), and utilitarianism.
Thomas Malthus's thesis focused on the biological and material limits to existence as the block to social, economic and other advancement. He was thoughtful but not ideological. Britain's subsequent population explosion shows that he failed to anticipate how newly emergent capitalism would release new technical energies and set new rules for production. Ironically, some of the most pointed criticism of his thesis came from Karl Marx (1818-1883) and Friedrich Engels (1820-1895), who emphasised that he failed to credit to capitalism's promethean technological dynamic, both in industry and in agriculture.
However, the Malthusian analysis resonated with emerging public health and later ecological thought. The 19th century birth control movement at one point identified itself as 'neo-Malthusianism'; mingling his ideas about family restriction with nascent feminism (he opposed contraception for religious reasons). Evolutionary biologists and naturalists Charles Darwin (1809-1882) and Alfred Russel Wallace (1823-1913) independently crystallised their ideas on natural selection after reading Thomas Malthus.
A century later, in the 1960s, the epidemiologist Thomas McKeown (1912-1988) argued that improved population health has little or nothing to do with medicine. It is due to 'rising standard of living, of which the most significant feature was possibly improved diet...' (22). He identified other drivers of health improvement as changes in social hygiene and sanitation, and the declining impact of the microbial disease environment
Many of the leading thinkers and doers in the fields of public health and nutrition in the 19th century were British. This was not by chance. Britain was the first nation to industrialise, and acquired a vast empire. The movement spread across the whole industrialising world, as philosophers, scientists, politicians and others engaged in thought and action, debated the consequences of mechanisation and urbanisation, and sought to frame new public policies and practices. Leading thinkers in Britain adopted utilitarianism, with its creed of the greatest happiness of the greatest number, to justify action on food and health. As a result, British governments set up controls to limit food adulteration, and introduced rigorous disease surveillance and public health surveys, including those concerning population nutrition. Other countries went different routes.
What went wrong?
Given all this, and given that nutrition is now once again understood as a key determinant of disease, health and well-being at all levels from global to personal, public health nutrition should now be central in public policies. All the more so, given the cost of treatment of related diseases. But to repeat, it is not.
Public health nutrition now is too often confined within a technical support role, administering or pursuing quick fixes for immediate public health problems. The profession is in danger of being absorbed into what we call the social-behavioural model of health. This makes the practice of nutrition quasi-scientific, operating on an individualised basis. In this model, governments abdicate their responsibility for public health, merely advocating what is now called the 'nudge' policy, in which consumers are 'nudged' to look after themselves better and industry is 'nudged' to do the right thing (23). Within this grossly inadequate and pathetic model, as evident now, public health nutrition programmes are more or less limited to 'soft' individualistic approaches, such as somewhat improved product labelling, or nutrition education, both of which are likely to be shaped to suit industry. The use of law and regulation is abandoned. This throws responsibility onto individuals, who are seen as mere consumers. It does not address the asymmetry of power.
The public health movement
It is sometimes supposed that the developments in public health that occurred in Britain and other European countries as they industrialised, were readily achieved – problems were recognised and therefore efficiently addressed. This was not the case. Much more than today, there was a ferment of debate, and positions were fiercely defended and attacked by rules, elites, vested interests and popular movements. Like today, the case for doing little or nothing was powerfully championed, filtered through a language of social class, laissez-faire philosophy and unwillingness to burden the State with new costs. Some said that workers chose to labour in dangerous factories, and that regulation was paternalistic. Others said that the existence of homeless, destitute and helpless people is a natural order of existence.
In those days the first task of the public health movement – its leaders really did see themselves as engaged in a social and political movement – was to make all classes of society listen, and then to convince them that the world of filth and ignorance could be transformed for the better.
Views of health now
Here lies the difficulty today, at least for those of us who live in economically wealthy parts of the world. Big, society-wide initiatives such as building sewage systems and piping clean water, seem set in the past or only needed far away. Or, if they are needed, they are solely for those at the margins of society, such as communities living in informal habitations, such as in remote rural areas or in caravans and trailers. It concerns 'them' not 'us'.
And, in any case, according to this attitude, the narrative has moved on from the environmentally-based diseases of the past. Aren't the new public health problems, such as drugs, alcohol misuse, bad diet, violence, matters of bad individual behaviour? People can therefore choose to avoid these exposures or, if the environment is so bad, they can leave. Go elsewhere. In discussions of public health in the last 200 years, and today, this mixture of moral elements can be detected.
The profusion of notions around health today amount to a babel of voices: how to be healthy, how to buy health, how to eat healthily, how to extend life, and so on. In societies driven by individualism, health becomes just another market opportunity, where economic wealth brings access to health clubs, medical care, designer food, information and education. But where does this lead? In the USA, the cradle of the ideology of individualism, one-third of the population is now obese, and two-thirds are overweight. People rarely choose to be fat. How is this explained? It generally isn't! There is a profound ideological mismatch between the model of health in people's minds and the reality of their bodies.
All over the world now, people are bombarded with messages about health. National histories, literature, television and radio shows, the internet, social networks, books, family histories, stories in newspapers and magazines, even song lyrics, all convey narratives about health. But note well, these are almost invariably about personal individual health, not about public health. The individual is the focus, usually far more than the family, and certainly more than the community or population. But public health certainly matters in a crisis. In the 2011 film Contagion a character played by Gwyneth Paltrow (in life, a health food enthusiast and colon cleanser: http://goop.com/) quickly succumbs to a new virulent bug, recalling the plague.
Today medicine is presented as supremely effective – providing that is, that you have the right physician or surgeon, with the right technology, at the right price. Yes, it's a myth, but one that most people seem happy to swallow. In 2008 the most watched TV programme in the world was the medical series House MD, an updating of Sherlock Holmes but relocated to a US hospital.
As with health generally, so it is with food and nutrition. The shaping of food systems and supplies with good nutrition in mind – commonplace in Europe in the 19th and first half of the 20th century, as witness the achievements of Justus Liebig (1806-1873) in Germany and John Boyd Orr (1880-1971) in Britain – has now been almost abandoned.
The meaning of health
So what does public health now mean, in most people's minds? More than a decade ago, the US Centers for Disease Control and Prevention (CDC), a government body, sought to find out. They undertook the study because ignorance was impeding their ability to make the case for effective public health policies and actions. Respondents were asked: 'When you hear the term "public health", what do you think of?' and then given a choice of four descriptions. More than half of the respondents did not see public health as either protecting the population from disease, or as policies and efforts that promote healthy living conditions. Yet when prompted and asked whether sufficient resources were being dedicated to public health, more or less two-thirds said that the government should do more. In a country saturated by images of hi-tech medicine, this is not surprising.
Enlightened ideas, policies and actions
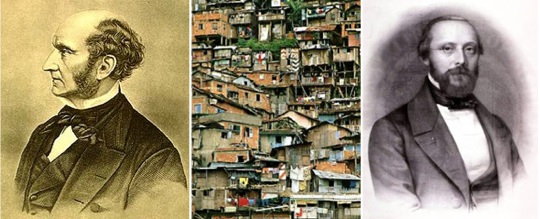
Outrageous living conditions cause malnutrition, a big 19th century issue for John Stuart Mill (left), Rudolf Virchow (right). A bigger issue now (centre)
It is sometimes supposed that the developments in public health that occurred in Britain and other European countries as they industrialised, were readily achieved – By contrast, in the mid-19th century, public health meant what the term says: the health of the public. By pairing the two words at that time, a new meaning and set of possibilities were created. Society could be changed for the better. Public health was a collective aspiration. It became expressed through new institutions and professions, sponsored by the State and also through civil society actions, social movements and also enlightened commercial policies and actions. Public health action clearly mattered then, because it was generally understood that it created healthier and more enjoyable or at least tolerable conditions of work and life. Public health generates public good.
Public health emerged as a social movement as part of the Enlightenment, which began in Europe and spread worldwide. It is said that Simon Bolivar, the greatest Latin American liberator from colonial rule, travelled with the books of three Enlightenment thinkers, Adam Smith, Voltaire and Montesquieu.
The philosophical grounding of the public health aspect of the Enlightenment was utilitarianism, a term coined by the political philosopher John Stuart Mill (1806-1873), and used to describe the ideas of the British legal philosopher Jeremy Bentham (1748-1832). The main early advocate of public health in the grand sense was Bentham's former secretary, Edwin Chadwick (1800-1890). JS Mill's message, as in his On Liberty (1859), was that people could be educated to think for themselves, that women could decide their own destiny, and that nature should be protected from avaricious capitalism. He declared that intolerable conditions of life should be abolished. Children need not die in infancy. The environment should be cleaned up. Food and water should be unpolluted. Workers should be protected (24).
Some 19th century leaders of the public health movement, such as Rudolf Virchow (1821-1902) in what became Germany, were even more radical than JS Mill. Most were less radical. Indeed, some measures introduced that were declared to be of general public benefit were repressive, such as housing clearances, population dispersals, and moralistic and punitive welfare. But the general effect was to slow down, check, and reverse the most vicious aspects of capitalism. These included many that have become rampant once again: chaotic urban growth, loss of human rights, ruthless employment practices – and food systems and supplies that are blatantly unhealthy. The main difference between then and now, is that now, public health, including public health nutrition, can hardly be described as a movement – certainly not one able, with mass public support, able to press governments and industry to change for the better. Again we ask, why is this?
The five models of public health
Here, in our view, is why. Here we briefly identify and describe first, the four current conventional models of public health. These all have shaped political, economic and social policies and population and personal behaviour. Everyone lives with all of them now. We then outline and advocate a fifth model.
Sanitary-environmental
This model focuses on the health of populations in their physical circumstances. It might equally be called the classical model of public health, for some of the measures with which it is associated are ancient, such as the laying of water pipes, sanitary engineering and the like. The Romans were its original masters.
In the 19th century, the challenge for this sanitary-environmental approach was to clean and clear up industrialisation's dirt and detritus – seen as the determinants of epidemic disease – and to rid society of nuisances to eye, ear and nose. Its advocates were known as sanitarians or hygienists. Its professionals were public health inspectors, engineers, town planners, building standards regulators, even street designers.
In the richer parts of the world today, these measures are taken for granted, so embedded as in effect to be invisible. Infrastructure is governed by tight rules and highly organised arrangements for managing human, biological and material flows and waste. Look elsewhere and a different picture emerges. In many of the new mega-cities populations far exceed the original physical arrangements – sanitation, power, clinical services, and so on, many times over. Such environments are the modern equivalent of early 19th century European cities.
Bio-medical
This model has a population orientation and also an individual orientation. Population based bio-medical interventions first came into prominence in the early 1800s with vaccination, and later through the establishment of public health laboratories. In its modern form, promoted by the English physician Edward Jenner (1749-1823), vaccination was claimed as more scientific, more effective and with fewer side-effects. (It had been in use in China for centuries previously). Vaccination rapidly caught on as national policy. Jenner was thanked not only by his home country but by the US president, despite poor vaccination techniques, compulsory use in poor communities, some adverse effects, and limited demonstration of effectiveness. Today vaccination has a powerful track record. In 1980 the World Health Assembly announced the eradication of smallpox. But vaccination retains a capacity to excite controversy, as was shown by the recent public concern in the UK over the triple vaccine for mumps, measles and rubella (25).
Bio-medical 'breakthroughs' continue to be the stuff of headlines. Now the shift has partly been to genetics. The 'wonder drugs' as so seen in the second half of the last century are losing their power. Antimicrobial drugs are grossly overused and abused and so have generated multiply drug-resistant strains of disease. The pioneers of antimicrobial discovery, who included René Dubos (1901-1982), understood evolutionary biology, and knew and warned of the risks, but the antibiotics and other antimicrobial drugs have been a bonanza for Big Pharma and have been overused and abused by physicians and in intensive rearing of animals, and these warnings were largely ignored until recently.
The personalised version of the bio-medical model continues to shape our understanding of how the human and living body works and fails to work. From the 1880s medicine began to cast aside ineffective treatments. It was only after the close of that century that, with the increasing use of aseptic techniques, post-surgical survival rates began to climb. After the Second World War progress has been exceptional, but comes with a warning, and at great cost.
For example, in the US in the 1950s, 4.4 per cent of gross domestic product (GDP) was spent on 'health care' – that is to say, the treatment of disease. William Schwartz of the Brookings Institution in Washington says that in those days, for a large percentage of patients, 'doctors really couldn't do much'. Since then the US has invested massively on devices such as the iron lung, the dialysis machine, the respirator, and computerised imaging. In 2009, 17.4 per cent of US GDP was spent on health care, almost double the high-income country average. By 2040 the level is expected to rise to close to 30 per cent (26).But at any amount of spending, medical technology does not alter the conditions in which rates of obesity and of serious diseases increase.
Social-behavioural
This model may seem new but it isn't. Rulers have attempted to influence the behaviour of their people for health reasons for centuries. King James of England and Scotland published a diatribe against tobacco in 1604. The model is older yet when religious precepts and commands that explicitly or implicitly include health, such as towards washing, or choice or preparation of foods, are included.
The social-behavioural model is now the main rival to the bio-medical model. It addresses the behavioural circumstances of health. Thus since the 1950s, food and nutrition, and physical activity, are increasingly seen as major factors in chronic disease and its prevention and control.
Here, public health is engaged with rules and guides to behaviour. But who makes these? The role of commerce is double-edged. In the 19th century, new mass-manufactured products were marketed with health messages. Ideas of personal health were changed, by messages such as the value of regular bathing of the bodies both of children and of oneself, about cleanliness of the home, and about women's domestic responsibilities and work. These were salutary. But the marketing firepower of transnational corporations whose ultra-processed products are in the quantities commonly or typically consumed, harmful to public health, is now massive. In work done for the World Health Organization, we have shown that Coca Cola spends more on its marketing of soft drinks than the entire budget of the World Health Organisation (27).
Ranged against the power of commerce, what leverage do public health advocates possess? What methods do they use? Is it psychology, marketing (with pitiful budgets)? Or is it law? Or do public health advocates ape the methods of commerce by employing social marketing or the latest fad, 'nudge'?
Techno-economic
The techno-economic model is central in the public health literature, while remaining until now unnamed and undesignated as a type. It depends on two concepts: economic growth, and knowledge growth.
One of its ideas is that economic growth, leading to a higher standard of living, leads to better nutrition. We are back with Adam Smith. Another idea is that knowledge growth and the conversion of knowledge into products, services, and energy-heavy living and work technologies, reduces physical stress on bodies and creates opportunities for easier, potentially richer lives. This is the view of Thomas McKeown.
In fact there is no automatic link between economic growth and better public health. This may be so, depending on other factors, such as effective institutions, limited corruption, the rule of law, reasonable levels of democracy. Nor does a cornucopia of choice of consumer goods provide the key to well-being. Beyond a point wealth certainly does not mean health. It may worsen health. Look at the rates of obesity in the US.
Conventional public health
What we mean by identifying these four models as conventional public health, is that they are already identified and implemented. They are conventional in other senses too. They engage with health in anthropogenic terms. The health of animals, except as used by humans, and of the whole living, natural and physical world, is basically ignored. Some environmental concerns may be lightly considered, but not at anything like the level that could improve the overall conditions of life (except of course for the relatively wealthy)
This was not how the public health movement began. In the mid 19th century it was well understood that cities depend for their sustenance in many senses of the word, on the countryside. Edwin Chadwick himself, with others, championed returning of organic detritus including human and animal faeces from the city to the land to improve it, an ancient practice in Asia, and now once again becoming current as a way to improve plant yield, mineral loss and sanitation. Health was considered within a biological and environmental context.
The fifth model: Ecological public health
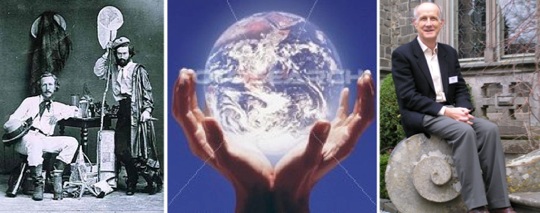
The one planet concept (centre): a big 19th century issue for Ernst Haeckel (left). The biggest issue in this century, as shown by Tony McMichael (right)
We now come to our main thesis. Here it is. All discussion of public health must encompass 'eco-systems health'. This is a reinvigorated and updated discourse around humans and the environment, a huge challenge for this century.
Figure 1
Human and eco-systems health

We express this as 'ecological public health', projected by the simple graphic shown as Figure 1, which is revolutionary in its implications. The concept also appears in the literature, but so far only at the margins, despite the support of influential public health bodies.
The challenge for this century is to work out the meaning and purpose of public health at a time of acute and critical threats to the environment, to eco-systems, and to the biosphere. The natural and physical world is not a limitless treasure of resources for human exploitation. The biological world cannot be ceaselessly and endlessly manipulated to human advantage. The prevailing debt-fuelled consumerist ideology cannot be sustained. It endangers human existence and the planet itself.
Ecological public health acknowledges a starting place in Malthus's analysis of human-environmental tensions. It adds a progressive, egalitarian outlook, with an updated and also critical view of the nature, purpose and limitations of science, evidence and scope for action. It also enters into discussion of the future.
It has been emerging, although not yet as a complete or considered model. One strand has been biological, as shown in worries about biodiversity loss or rising antimicrobial resistance which makes drugs ineffective. Another has a material basis in the link between industry, energy use and toxicity, with a double impact, on the human species and on the rest of nature. A third strand is cultural and societal. Ecological thinking has now extended far beyond its early traditions, before, during and after the period dominated by Social Darwinists (whose philosophy was much more dogmatic that anything Charles Darwin himself wrote), with their specious and pernicious speculations on human differences. Indeed there is a growing interest in the progressive strands of early Darwin-influenced philosophy, science, psychology, and economics, such as found in the thinking of Charles Sanders Peirce (1839-1914), William James (1841-1910), GH Mead (1863-1941), and Thorstein Veblen (1857-1929).
Modern ecological thinking is able to face complex and dynamic biological, material, social and cultural dimensions of the human, living and physical world. It works better than other models in a number of ways:
- It draws upon conventional models and plays to their strengths.
- It is the one model of the five that is fully integrative.
- It draws upon complexity science and system dynamics, addressing, for example, questions of non-linearity, variations in scale, feedback, and other emergent qualities of nature and human behaviour.
- It seeks to build knowledge, not just a narrow 'evidence-based' perspective.
- It incorporates evolutionary thinking, from matters like nutritional mismatch to questions of biological feedback.
- It engages multi-actor engagement: action is required by all.
- It is interdisciplinary, not simply built around tiered and unequal multidisciplinary compartments.
- It is inter-dimensional, incorporating the material, biological, social and cultural dimensions of life.
The last point on this list is a new conceptual development. Public health needs to address what we term the four dimensions of existence. These are:
- The material dimension. The physical and energetic infrastructure of existence (matter, energy, water), the physical building blocks on which life depends.
- The biological dimension. The bio-physiological processes and elements This includes all animal and plant species and also microorganisms.
- The cultural dimension. How people think and through what mental categories, the sphere of interpersonal relationships, community, group and family traditions.
- The social dimension. Institutions created between people and expressed in terms of laws, social arrangements, conventions, and the framework of daily living generally outside of individual control.
Policies and actions should be designed to engage with each of these dimensions. Thus, programmes of behaviour change designed to improve nutritional status, whether for people, communities or populations, will not work if they are limited to what people know or think they know, and do not understand, and as needed change, the material or social character of the context in which they live. Telling families who live in deep poverty that they should make sure to eat well every day is insulting and futile.
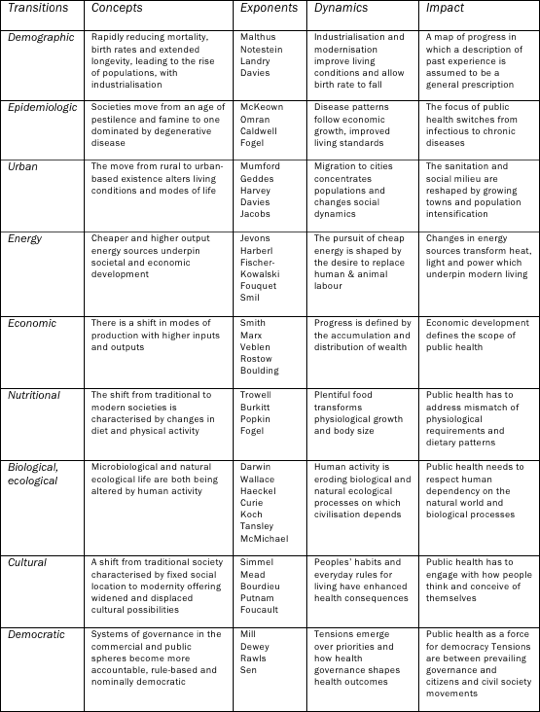
Transitions
Change is a natural state of affairs. It is the essence of species evolution. Changes in human affairs over the last half century alone have been astounding. The world of the early political economists, over two centuries ago, was dominated by sparse, relatively static food choices modified by limited trade and population movement. Today fruit is air-freighted and containerised. Supermarkets are crammed with many thousands of branded ultra-processed products engineered in laboratories. The overall energy used every day to support the lives of people in high-income countries would have been enough for a year or much more, 200 years ago. And so on.
Ecological public health has to take a long view, back in history fully to understand where we have come from, and forward well into the future. It will be wise to think into the next century. In our new book, and as shown in Table 2, we list the key writers, encapsulate the key ideas, and identify and describe nine transitions that have, do and will shape conditions for interaction between humans and ecosystems. These are
• Demographic
• Epidemiologic
• Urban
• Energetic
• Economic
• Nutritional
• Bio-ecological
• Cultural
• Democratic
The democratic transition is that in which conditions of existence are shaped by an informed, participative and critical public. This is another lesson of the Enlightenment.
Table 2
Transitions that shape public health:
their concepts, exponents, dynamics, and impact
We take 'ecology' to refer to the concept that everything in life is interconnected. Hence our core model shown as Figure 1. The task of ecological public health is to identify the key relationships and connections, to preserve and develop those that respect and protect the planet and all that is in it, and to change those that are evidently damaging or malignant.
Ecology is not just about botany and biology. It is about the material world, and society and culture too. In this century public health needs to identity and address the four dimensions of existence.
Where does public health fit, within current sustainable development thinking? It is hard to say. The main tradition of sustainable development, enshrined at the 1992 Rio Earth Summit – to be revisited in Rio this June – includes three 'pillars'. These are social, economic, and environmental (28).
Health cuts across all three. But it tends to be confined to the 'social' pillar. As a result, policies and practices concerned with sustainable development are weak on health. Work tends to focus on the environment without people, or else to be reduced to economic arguments about rising wealth, healthcare costs and investment patterns, a trade-off of investment and risks.
The model is wrong. In contrast, ecological public health relocates health firmly within what can broadly be termed the Darwinian tradition of scientific thinking. For Charles Darwin, and later for Ernst Haeckel (1834-1919), who coined the term 'ecology', it was about the 'web of life' – but without humans. Today we know better, and the full concept of what ecology really means has been wisely articulated by thinkers, writers, speakers and campaigners like René Dubos and Tony McMichael (1942- )(29,30).
Ecological public health nutrition
So, what about public health nutrition, within this ecological framework? We certainly are proposing that it should take account of sustainability. Here is one example: dietary guidelines. Food-based population dietary guidelines must now be revised, to become sustainable. Do we eat more fish? Yes, nutritionists continue to say. No, say environmentalists, or at least only fish from sustainable stocks. But sustainable for everybody? Really? How could the 7 billion, or the 10 billion, be fed with more fish?
But the issues are also far wider. Happily, ecological public health thinking directly translates into public health nutrition. Indeed, arguably they only differ in focus. They share many concepts, assumptions and goals.
Seen from the ecological point of view, the 'public health imagination' is in part a restatement of the original, investigative, forward-looking perspective of the early modern public health movement. As from the early 19th century this embraced what is now identified as 'public health nutrition'. It dared to believe and to act on the belief that reality can be altered, and common policies and practices can be confronted or reshaped.
The bases for policies and actions
Public health thinking needs to be constantly refreshed and updated. This is not just a matter of mining and sifting evidence. It also needs production of new hypotheses, engaging what C S Peirce150 years ago called 'abductive' reasoning, which begins with an idea (31). This is how ecological thinking began, by a continual process of sifting, observing, theorising, postulating, testing. Properly understood, it is also how science has developed.
Ecological public health seeks knowledge that is not merely application of evidence from interventions and other experiments, with the restrictions and passivity which this approach entails. Public health cannot be reduced to only that which is already 'evidence-based'. This colludes with the status quo. Restriction to 'evidence-basis' is also naïve: knowledge growth, and social development, has always and will always operate through more dynamic evidential parameters.
Public policy works either with partial evidence, or despite it, or in the face of it. Yes, it is important to strengthen evidence, but there is no such thing as a perfect state of evidence. There never will be. Public health decisions and actions have always and will always be made and carried out in a context of contested evidence, ignored evidence, rediscovered evidence, right evidence with the wrong theory, wrong theory with the right evidence, evidence gathered without policy consequences or, perhaps the best kind, slow-burning evidence.
Being able to assess evidence and refresh concepts by scientific endeavour is of huge value. But progress in public health cannot rely on scientific evidence alone. It also requires thought. Judgements and actions in public health simply cannot be the responsibility of single-issue, expert-led professions. There must be access to a wide range of different types of knowledge and understanding, including and beyond the natural sciences. This includes listening to the people who most suffer from bad public health conditions who, partly for this reason, are unlikely to be well educated. But they suffer the direct experience, and are knowledgeable. Epidemiology, the use of statistical modelling and other forms of mathematically-based reasoning, are all part of that project. But epidemiology alone cannot be the sole or main basis in public health – including public health nutrition – policies and actions.
Institutional renewal
Institutions that impact on public health need revision and renewal. These include organisations and agencies, ways of working, the deployment of professionals, and the outlook and ambitions of the institutions as a whole.
The public health institutions in place now are mostly a legacy of 19th and early 20th century public policies and practices. Whether international, national or municipal, they are fractured, arbitrarily divided across sectors. How can public health nutrition be addressed coherently at UN level, for example, when the World Health Organization, the Food and Agriculture Organization, the UN Children's Fund (UNICEF), the World Food Programme, the International Labour Office, and other UN agencies, often or usually with different or conflicting precepts, policies and practices, all have their fingers in the pie? It is highly significant that the UN System Standing Committee on Nutrition, set up specifically to co-ordinate all 19 UN agencies whose work touched of food and nutrition, now apparently lies in ruins.
The UN agencies have become more marginal over time, not least because the Bretton Woods global financial institutions (the World Bank, the International Monetary Fund) and now the World Trade Organization and the World Economic Forum, which are mainly concerned to promote bigger business, are much more powerful. Set up in the 1940s, the UN agencies have been further fragmented by 'bolt-on' new organisations alongside. A total overhaul of the UN system as it affects public health – and other crucial areas of public policy – is essential.
Renaissance
The 20th century fantasy of endless resource and limitless choice is over. Yet it persists and remains forceful in wealthy countries, and is a compelling driving force in countries many of whose people are making more money. Cities in Asia and Africa are jammed with cars. And here is a trap for public health advocates. In pointing out the dark side of consumerism, and of car culture – which distorts physical activity and invents new food supply systems, with the rise of hypermarkets and cheap calories – and the rising impact of chronic disease, public health champions are often seen as authoritarian impeders of freedom and the good life.
This must be countered. Public health advocacy is engaged in the revival of culture, the enjoyment of imagination, and the promotion of real communities in cities and the countryside, and of human creativity. Health – remember that the roots of the word link with concepts of the holy and wholeness – should be explored, developed, achieved as a central and binding part of all societies.
Ecological public health dissolves compartmentalised thinking and false divisions. There is no schism between politics and public health nutrition, which is both a science and a movement. It embraces natural and social science. It is about people, and the planet
Conclusion
Big problems in public health are usually systematic. They have always required systems thinking, even if such thinking is resisted. This involves ecological, multi-level, multi-sector analyses and responses. We believe that what we term 'ecological public health' is the way through this complexity. Seeing it as the culminating great traditions of public health thinking – all of which have nutritional aspects, all with champions – explains where history has led us.
Ecological thinking should unify and extend the relationship between knowledge, policy and action, and indeed the ways in which we live, including around food. Its vision works in our times and in response to current threats. It provides an intellectually omnivorous conceptual framework, for thought and action. No one outlook or profession or discipline is on top; all have potential value. Public health seen as an ecological discipline provides a strong and resilient intellectual framework for defining and developing the politics of health. Rally round it.
References
- Winslow C.-E. The Untilled Fields of Public Health. Science 1920. 51(1306).
- Vernon J, Hunger: a modern history. 2007, Cambridge MA: Harvard University Press, 2007.
- Monteiro C. The big issue is ultra-processing. World Nutrition 2010. 1(6), 237-269.
- Organization for Economic Cooperation and Development/International Energy Agency, Biofuel Support Policies: An Economic Assessment. OECD/IEA: Paris, 2008.
- United Nations Environment Programme/GRID-Arendal. The Environmental Food Crisis: The Environment's role in averting future food crises. A UNEP rapid response assessment. 2009, UNEP/GRID/Arendal, Norway, 2009.
- United Nations Department of Economic and Social Affairs. World Economic and Social Survey 2011: The Great Green Technological Transformation. http://www.un.org/en/development/desa/policy/wess/wess_current/2011wess.pdf New York, 2011.
- Stern, N., The Stern Review of the Economics of Climate Change. Final Report. HM Treasury: London, 2006.
- Tukker Anet al., Environmental Impacts of Diet Changes in the EU. Seville: European Commission Joint Research Centre Institute for Prospective Technological Studies, 2009.
- Steinfeld H. et al., Livestock's Long Shadow: Environmental Issues and Options. Rome: Food and Agriculture Organization of the United Nations, 2006.
- Millennium Ecosystem Assessment (Programme), Ecosystems and Human Well-being : Synthesis. The Millennium Ecosystem Assessment series. Washington, DC: Island Press, 2005.
- World Wildlife Fund. Thirsty Crops: Our Food and Clothes: Eating up Nature and Wearing out the Environment? WWF: Zeist (NL), 2006.
- Chapagain A, Hoekstra A. Water Footprints of Nations, vols. 1 and 2., in UNESCO-IHE Value of Water Research Report Series No. 16. Paris: UNESCO, 2006.
- Food and Agriculture of the United Nations. Dimensions of Need: an Atlas of Food and Agriculture. Rome: FAO, 1995.
- Food and Agriculture Organization of the United Nations. State of Food and Agriculture 2007. Rome: FAO, 2007.
- World Economic Forum and McKinsey. Realizing a New Vision for Agriculture: A Roadmap for Stakeholders. World Economic Forum: Davos, 2010.
- GAIN, Global Alliance for Improved Nutrition (GAIN) Business Alliance. http://www.gainhealth.org Global Alliance for Improved Nutrition: Geneva, 2012.
- Marmot M, Fair Society, Healthy Lives. Final Report of the Strategic Review of Health Inequalities in England Post 2010. University College London: London, 2010.
- Lang, T, Barling D, Caraher M, Food Policy: Integrating Health, Environment and Society. Oxford: Oxford University Press, 2009.
- Burnet E, Aykroyd W Nutrition and public health. Quarterly Bulletin of the Health Organization (forerunner of WHO), 1935. 4(2): June.
- Smith A. The Wealth of Nations. London: Penguin, 1970. (First published 1776).
- Malthus T. An Essay on the Principle of Population, as it Affects the Future Improvement of Society with Remarks on the Speculations of Mr Godwin, M Condorcet and Other Writers. First edition. London: Printed for J. Johnson, 1798
- McKeown T. Medical issues in historical demography. In Clarke E (ed). Modern Methods in the History of Medicine.. London: Athlone Press, 1971.
- Thaler, R, Sunstein C, Nudge: Improving Decisions about Health, Wealth, and Happiness. New Haven CT: Yale University Press, 2008.
- Mill JS. On Liberty. Kitchener, Ontario: Batoche Books, 2001. (First publishes 1859).
- Godlee, F, Smith J, Marcovitch H, Wakefield's article linking MMR vaccine and autism was fraudulent. British Medical Journal 2011. 342: c7452.
- Fogel R. Forecasting the cost of US health care in 2040. In: NBER Working Paper No. 14361. Washington DC: National Bureau of Economic Research, 2008.
- Lang T, Rayner G, Kaelin E, The Food Industry, Diet, Physical Activity and Health: a review of reported commitments and practice of 25 of the world's largest food companies. London: City University Centre for Food Policy, 2006.London.
- UNCED, Rio Declaration, made at the UNCED meeting at Rio de Janeiro from 3 to 14 June 1992. United Nations Conference on Environment and Development: Rio de Janeiro, 1992.
- Dubos R. Man Adapting. New Haven, Conn: Yale University Press, 1965.
- McMichael AJ. Human Frontiers, Environment and Disease. 2001, Cambridge: Cambridge University Press, 2001.
- Buchler J (ed). Philosophical Writings of Peirce. Mineola, NY: Dover Publications, 1955.
Acknowledgement and request
Readers may make use of the material in this commentary if acknowledgement is given to the Association, and WN is cited
Please cite as: Rayner G, Lang T. Public health and nutrition. Our vision: Where do we go? [Commentary] World Nutrition, April 2012, 3, 4: 92-118. Obtainable at www.wphna.org
The opinions expressed in all contributions to the website of the World Public Health Nutrition Association (the Association) including its journal World Nutrition, are those of their authors. They should not be taken to be the view or policy of the Association, or of any of its affiliated or associated bodies, unless this is explicitly stated.