World Nutrition
Volume 2, Number 6, June 2011
Journal of the World Public Health Nutrition Association
Published monthly at www.wphna.org
The Association is an affiliated body of the International Union of Nutritional Sciences For membership and for other contributions, news, columns and services, go to: www.wphna.org
Commentary.Prevention of obesity
Finding the best evidence


Shiriki Kumanyika (corresponding author)
Department of Biostatistics and Epidemiology, and Department of Pediatrics
(Gastroenterology; Nutrition Section)
University of Pennsylvania School of Medicine, Philadelphia, PA, USA
skumanyi@mail.med.upenn.edu
Christina Economos
Friedman School of Nutrition Science and Policy
Tufts University. Boston, MA, USA
Introduction
A crucial public health task is to check and even reverse the current pandemic of overweight and obesity (1-4). The epidemic would not abate, even were perfect and long lasting treatments to become available tomorrow. Treatment of those already obese cannot stop the new development of obesity in children and adults in the population at large, as long as the societal factors that lead to excess weight gain are in force.
The World Health Organization (WHO) has estimated that in 2005, approximately 1.6 billion adults (age 15+) and 20 million children, were overweight or obese, and at least 400 million adults were obese. Projections are alarming: 2.3 billion adults overweight or obese, and 700 million obese by 2015 (5). Once considered a problem only in high-income countries, overweight and obesity are also problems in many low- and middle-income countries. The scope of the problem is underscored by a recent analysis of global trends in body mass index between 1980 and 2008, based on data from 199 countries and territories (6).
At a broad conceptual level, what needs to be done to prevent obesity is clear (1, 2). Strategies are needed to block or circumvent societal pathways that predispose people in general to excess weight gain and to create and render normative environments that facilitate achievement of appropriate population weight levels. However, the clarity implied by broad statements about needed actions, turns to uncertainty and controversy when trying to pinpoint specific ways to intervene.
The pathways of interest involve core societal structures and processes that are interrelated and ever-changing, and have multiple beginning and end points. Furthermore, the aspects of society involved – for example, the market economy, agricultural products, global food companies, trade policies, marketing to children, community design, impacts of technology, and the socio-cultural nature of food and eating – involve powerful entities and are formidable targets in many respects.
Given the scope and health and economic consequences of the obesity epidemic, the option of not taking preventive actions is untenable; but evidence to inform decisions about which actions to take and how to formulate and implement them is quite limited (7) . Moreover, agreement about the type of evidence that can be helpful and how to identify or obtain it, is lacking both among potential users and among researchers who might contribute such evidence.
The type of evidence to which we are accustomed, may relate to studies with a single focus, generated by academic researchers who exercise as much control as possible when conducting the studies. Such studies may be viewed as very convincing when judged by the typical evidence hierarchy, but they may be uninformative with respect to what takes place in real world settings. Furthermore, the type of evidence that is available may have been geared to answer questions posed by researchers, or with no guarantee of relevance to decision makers. This evidence gap creates tension between the sense of urgency to take action to prevent obesity and the lack of specificity about what actions to undertake.
The need for bold steps to close this evidence gap was the focus of an Institute of Medicine (IOM) study committee report released in April 2010 (8). The committee was convened because a lack of consensus on evidence standards related to obesity prevention, including some concerns about the value of systematic reviews in this domain, had been identified as an impediment to progress in addressing the obesity epidemic (4, 9-11). Also, the debate about evidence in obesity prevention was recognised as part of an ongoing international discourse about the need for greater clarity and creativity regarding evidence to inform policy and environmental change initiatives in public health and health promotion (12-25).
The IOM committee proposed a new evidence framework. This commentary is authored by the study committee chair (SK) and one other committee member (CE), both members of the public health nutrition community. It is intended to draw attention to the committee's findings and recommendations, and to motivate consideration and ultimately adoption, of the framework's perspective and approach.
Evidence: Taking a broader perspective
The process
Appropriate to the scope and complexity of the issues, the IOM convened a 16-member study committee with expertise that included public health, public policy, economics, systems thinking, programme implementation, and general community prevention research, as well as nutrition, physical activity, and obesity prevention research and interventions specifically, and methodological experts in biostatistics, epidemiology, biomedical evidence hierarchies, evaluation and social science research.
Over a period of about 18 months, these experts deliberated at face-to-face meetings and teleconferences, obtained information at two public workshops, and drew upon the findings and conclusions of a number of prior reports and other resources related to evidence-based public health and public policy. The focus was on the context for obesity prevention in the United States, but information gathering took a global perspective. The process was supported by a highly qualified staff and by an extensive review of relevant information, information resources, and related endeavours. An initial draft of the report was submitted by the IOM to a selected group of 13 external experts in relevant areas of research, policy, and practice for an independent, rigorous peer review. The result is explained in a well-referenced and indexed report of approximately 300 pages that includes an executive summary and several appendices (8).
Two concurrent activities were undertaken to assess the scope and nature of the problem and identify needs to be addressed by a new framework. One was a critical review of the evidence base. This took the form of a secondary review of approximately 50 published appraisals of evidence for obesity prevention published during the prior 13 years, a period characterised by major attention to the obesity epidemic in the scientific literature and the media. These appraisals included meta-analyses, systematic reviews, integrative reviews, reviews of reviews, evidence syntheses, best practice summaries, and task force recommendations.
Findings
Authors of appraisals had identified as few as 12 and as many as 13,000 potentially relevant studies, of which a much smaller number (3 to 158) met the relatively narrow inclusion criteria these authors had applied. The apparent lack of evidence for effectiveness was compounded by a strong focus on physiological outcomes (body mass index or body fatness) likely to be unaffected by policy level or programmatic interventions with a single focus. The lack of informative studies was especially troubling given the large amount of research published on obesity and even on aspects of obesity prevention. Reviews that adhered to the extant conventions about systematic reviews were not particularly helpful.
Among the problems identified with these reviews were the lack of clear conceptual frameworks for evidence selection, the dearth of research on community, environmental, and policy-based obesity prevention initiatives, and the limited attention given to reporting information about how these approaches might work in the real world. Studies included in many of the reviews overlapped, although conclusions varied. In general researchers reviewing this type of evidence found very little good quality evidence based on conventional criteria, and studies rated as high quality were often inconclusive as to what might work. This confirmed the impression that the current research literature lacks the power to set a clear direction for obesity prevention across a range of target populations.
Foremost among challenges to be addressed by a reframing of the evidence paradigm were:
- The need to free up population approaches to obesity prevention from being viewed through a clinical lens, and from a sense that evidence needs can be best served by a single type or hierarchy of evidence.
- The need to incorporate rather than ignore the inherent complexity involved in addressing the multiple influences on eating and physical activity patterns in populations.
- The need to give priority to both certainty (internal validity) and relevance to context (external validity, cost, transferability, sustainability).
The L.E.A.D framework: A new approach
Key issues and audiences
The committee oriented its deliberations about framework development by considering a range of potential decision-making scenarios of potential relevance to multi-level and multi-sectoral obesity prevention, with two overarching questions:
- How can relevant evidence that is currently available at any given time be identified, evaluated, and compiled to inform decisions about obesity prevention?
- How can more evidence be developed that is both high quality and user-oriented, that is, directly relevant to obesity prevention decision-making?
Consistent with these questions, the major user groups to focus on in developing a new framework were:
- Decision makers in policy and programmatic settings relevant to obesity prevention – where relevance was defined broadly to include the spectrum of influences on population eating and physical activity patterns.
- Academic researchers and others who generate evidence that could be useful for informing obesity prevention decisions.
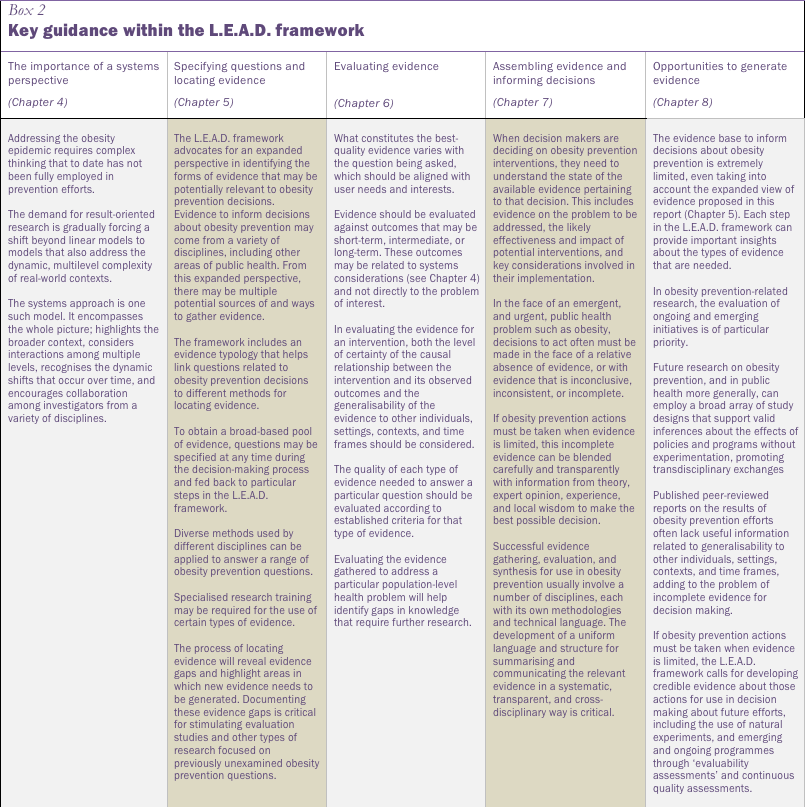
Framework elements and guidance
The proposed new framework is shown graphically in Box 1, with associated key guidance highlighted in Box 2. The acronym, L.E.A.D., is short for Locate evidence, Evaluate it, Assemble it, and Inform Decisions. It also implies the intention to lead the obesity field in new directions. The framework enhances the basic process for compiling and evaluating evidence by introducing specific principles, concepts, and resources. The steps or phases build on the traditional process, but are predicated upon a new, more inclusive and transdisciplinary way of thinking about the nature of the task and the execution of each step.
L.E.A.D. is offered as a framework for improving the use and availability of evidence to inform decisions, rather than as a decision making framework. This is realistic and appropriate in the face of the numerous predispositions and contextual factors that influence decision-making as well as the many ways in which evidence is positioned within these processes (26, 27). For simplicity, the arrows are shown as unidirectional, suggesting linear progression. However, the process itself is inherently iterative and meant to encourage and benefit from feedback among different steps.
Box 1The IOM L.E.A.D. framework
|
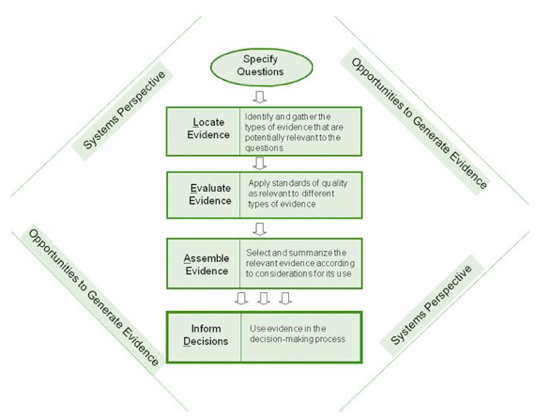
|
This process does not provide short-cuts in using evidence, and also does not lower the standards for evidence quality. Rather, it seeks to improve the process by focusing evidence-gathering and use on potential solutions to the obesity epidemic that may take a variety of forms. The framework broadens the scope of what is considered to be useful evidence and advocates for matching evidence to well-specified, user-oriented evidence needs. It reaffirms the importance of validity and reliability. but points out the fallacy of judging these in the same fashion across all types of evidence and without regard to external contexts.
As shown in Box 2, below, the first (chapter 4) and last (chapter 8) chapters in a five chapter sequence emphasise cross-cutting principles: the importance of taking a systems perspective, and the importance of vigilance for opportunities where new evidence would be informative.
Chapter 4 explains the concept of systems thinking with examples of how this can be interpreted in obesity prevention. Chapter 8 reviews the importance of generating more, and more useful, evidence and is supported by an appendix that provides an in-depth look at potentially relevant study designs and methodologies for simultaneously addressing rigor and relevance. Chapters 5 through 7 explain how the process of finding, using, and assembling evidence can be enhanced by clearer specification of questions, broader and more transdisciplinary perspectives on evidence, and systematic, transparent conventions for reporting results of the evidence gathering process. Chapter 5 provides a typology to differentiate among potential user questions (referred to as Why? What? and How? questions) and explains the respective implications for information inputs, use of qualitative and quantitative study designs and analyses, and reporting details. Chapter 5 is supported by an appended listing of leads to information across a broad spectrum: scientific literature databases covering multiple disciplines, and grey and unpublished literature; surveys, polls, rankings; government reports; and compilations of policies and programmes. Chapter 6 identifies guidance for understanding quality standards for evaluating different types of evidence in terms of both certainty and relevance to specified outcomes. Chapter 7 suggests a uniform template for transparent reporting of results of the information gathering process and also discusses principles for making informed decisions in the face of incomplete evidence.
Recommendations
Recommendations in the final chapters of the report promote the use and dissemination of the L.E.A.D. framework by identifying essential actions needed to generate adoption and utilisation of the main principles and concepts (see Box 3). They encourage refinement of the framework through an ongoing dialogue among users. Various recommendations are addressed to decision-makers and researchers themselves and, perhaps more fundamentally, to other audiences that have a major impact on the attitudes and behaviours of decision-makers and researchers and the contexts in which they function – such as government and private research funders, academic institutions, educators, scientific journal editors, and professional organisations.
Box3
Recommendations for disseminating
the L.E.A.D framework
| What? | Who? |
|---|---|
Apply the L.E.A.D. framework as a guide in the utilisation and generation of evidence to support decision-making for complex, multifac¬torial public health challenges, including obesity prevention. |
Decision-makers and those involved in generating evidence, including researchers, research funders, and publishers of research |
Incorporate systems thinking into research-related activities. |
Researchers, government and private funders, educators, and journal editors |
Build a system of resources (such as people, compendiums of knowledge, registries of implementation experience) to support evidence-based public policy decision-making and research for complex health challenges, including obesity prevention. Catalyse and support the establish¬ment of guidance on standards for evaluating the quality of evidence where such stan¬dards are lacking. |
Government, foundations, professional organisations, and research institutions |
Consider the inclusion in research studies of a focus on the generalisability of the findings and related implementation issues at every stage, from conception through publication. |
Obesity prevention research funders, researchers, and publishers |
Increase opportunities for those carrying out obesity prevention initiatives to measure and share their outcomes so others can learn from their experience. Encourage collaboration among researchers in a variety of disciplines so as to utilise a full range of research designs that may be feasible and appropriate for evaluating obesity prevention and related public health initiatives |
Research funders |
Bring together researchers, research funders, publishers of research, decision makers, and other stakeholders to discuss the practical uses of the L.E.A.D. framework and to develop plans and a timeline for focused experimentation with the framework and for its evaluation and potential refinement. |
A public-private consortium |
Gaining traction
Report visibility
Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making was released on 23 April 23 2010 in pre-publication form, and published in final form six months later. At the time of release, five committee members presented the report to a diverse public audience and answered questions at a teleconference that was joined by more than 200 unique listeners. Several organisations issued e-mail and web announcements about the report shortly after its release.
The timeliness of the report was linked to concurrent discussions about major funding for prevention and prevention research initiatives and also to the high profile Let's Move child obesity prevention campaign launched by First Lady Michele Obama a few months prior (28). Just days after the report's release, it was cited in a letter sent to the US Secretary of Health and Human Services by prominent advocacy organisations, calling for prioritisation of 'interdisciplinary, multi-field strategies and policies in the new wave of public health funding' (29).
Within 10 months, the report landing page on the IOM website had been viewed by approximately 8,400 unique visitors. The 4-page report brief had been downloaded more than 2,300 times, and approximately 250 copies of the report had been purchased from the National Academies Press website. To date the report has already been cited at least five times in scientific journal articles that advocate for or explain inclusive evidence uses for policy and program evaluation, including a commentary in the American Journal of Epidemiology by one of the committee members (30-34).
Early conversations
The committee chair's July 2010 presentation to the steering committee of the National Collaborative on Childhood Obesity Prevention (NCCOR)(35) was among the first opportunities to discuss the report and its implications with a broadly based set of key stakeholders in the research funding arena. NCCOR members include two of the three report sponsors (the Robert Wood Johnson Foundation and the Centers for Disease Control), several entities within the National Institutes of Health, as well as the United States Department of Agriculture.
The report has also been presented directly to hundreds of key stakeholders and potential users at scientific and professional meetings including the Federation of American Societies for Experimental Biology, Society for Prevention Research, American Association for Cancer Research, Association of State and Territorial Health Officials, American Public Health Association, American Evaluation Association, and—to reach an international audience—the European Association for the Study of Obesity. Other presentations have been made in educational settings and to editorial boards of scientific journals.
Conclusions
The public health nutrition literature reflects several arguments put forth to support the notion that modification of the existing 'levels of evidence' and grading systems used in clinical medicine is needed for use in prevention (12).
There continues to be agreement that scientific evidence (best available) should inform decisions (16) and that a rational approach should be followed to evaluate the evidence. But there is concern that methods used to review, evaluate and summarise evidence still have their roots in giving preference to randomised controlled trials. Because RCTs are inappropriate for many lifestyle interventions, community-based trials and societal/social change interventions, research on these types of interventions is often omitted from the traditional reviews that generate recommendations, guidelines and standards (12, 36, 37).
Also, the preponderance of evidence on interventions at the individual level rather than the population level may distort the conclusions reached and perceptions of policy makers about how to proceed. Overall, this leaves the field somewhat muddled, uncomfortable and unable to take action even in the face of need and crisis.
The evidence base has improved in recent years, but lack of consensus on which types of evidence will be viewed as credible and legitimate remains. The L.E.A.D. framework grew out of a need to shift thinking in the field. Its purpose is to create an authoritative break with the rigidity of the ways that hierarchies of evidence evaluation are applied, and to open the door for modifying views of evidence, going beyond prior efforts in this realm by describing a comprehensive process that has flexibility and adaptability.
The key question at this juncture is whether the IOM voice on evidence for obesity prevention will be sufficiently influential in a world dominated by the perception that good science is defined only by considerations that apply to medical-surgical treatment of individuals. The answer to this question will depend on the extent to which the framework is embraced, used, and disseminated by influential stakeholders. If the answer is 'yes', benefits for obesity prevention will be synergistic with those that extend to public health more broadly. The further articulation of an identity for evidence-based public health that is as equally respected as, but separate from, that for evidence-based medicine, will encourage the unapologetic use of the full range of information sources and methodologies appropriate to the potential solutions and contexts of interest.
Evidence issues that relate to creating dietary guidance, such as using science to determine what people should eat, fall outside the domains addressed by the L.E.A.D. framework, which is intervention oriented. However, the emphasis on systems perspectives, the cautions about narrowly framed outcomes and systematic reviews, and the importance of using methodological approaches that can account for complexity, is critical across nutrition and many other scientific domains (38, 39).
Our impression is that the report has been very well received, and even seized upon in some instances to bolster ongoing arguments that could benefit from a timely, authoritative, and detailed reference in the evidence literature making the case for a new paradigm. This is encouraging, but we recognise that the process of a research culture change of the magnitude called for in this report began a while ago, and needs time to evolve.
Impact of the report can be accelerated if influential champions step forward to promote its consideration and use and if the infrastructure needed to support its use emerges. Adoption will also be increased if the report's conceptual inspires the next generation of public health and policy scholars who have a hunger for societal change to take a systems perspective and a broad, interdisciplinary view of what constitutes 'evidence'.
Acknowledgements
References
- World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser, 2000,894:i-xii, 1-253.
- Kumanyika S, Jeffery RW, Morabia A, et al. Obesity prevention: the case for action. Int J Obes Relat Metab Disord, 2002,26:425-36.
- Friel S, Chopra M, Satcher D. Unequal weight: equity oriented policy responses to the global obesity epidemic. BMJ, 2007,335:1241-3.
- Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation, 2008,118:428-64.
- World Health Organization. Obesity and overweight. Retrieved February 2, 2011 from http://www.who.int/mediacentre/factsheets/fs311/en/index.html., 2006. (http://www.who.int/mediacentre/factsheets/fs311/en/index.html).
- Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet, 2011,377:557-67.
- Must A, Hollander S, Economos C. Childhood Obesity: A growing public health concern. Expert Rev Endocrin Med, 2006,1:233-54.
- Institute of Medicine. Bridging the Evidence Gap in Obesity Prevention. A Framework to Inform Decision Making. Washington, D.C.: The National Academies Press, 2010.
- Swinburn B, Gill T, Kumanyika S. Obesity prevention: a proposed framework for translating evidence into action. Obesity Reviews, 2005,6:23-33.
- Institute of Medicine. Progress in Preventing Childhood Obesity. Washington, D.C.: National Academies Press, 2007.
- Institute of Medicine. Preventing Childhood Obesity. Health in the Balance Washington, D.C.: The National Academies Press, 2005.
- Kroke A, Boeing H, Rossnagel K, et al. History of the concept of 'levels of evidence' and their current status in relation to primary prevention through lifestyle interventions. Public Health Nutr, 2004,7:279-84.
- Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services - Methods. American Journal of Preventive Medicine, 2000,18:35-43.
- Waters E, Petticrew M, Priest N, et al. Evidence synthesis, upstream determinants and health inequalities: the role of a proposed new Cochrane Public Health Review Group. Eur J Public Health, 2008,18:221-3.
- Victora CG, Habicht JP, Bryce J. Evidence-Based Public Health: Moving Beyond Randomized Trials. American Journal of Public Health, 2004,94:400-05.
- Margetts B. Making Public Health Nutrition relevant to evidence-based action: are we doing enough? Public Health Nutr, 2001,4:1199.
- Margetts B, Warm D, Yngve A, et al. Developing an evidence-based approach to Public Health Nutrition: translating evidence into policy. Public Health Nutr, 2001,4:1393-7.
- Kellam SG, Langevin DJ. A framework for understanding "evidence" in prevention research and programs. Prevention Science, 2003,4:137-53.
- Green J, Tones K. Towards a secure evidence base for health promotion. Journal of Public Health Medicine, 1999,21:133-39.
- Petticrew M, Cummins S, Ferrell C, et al. Natural experiments: an underused tool for public health? Public Health, 2005,119:751-7.
- Petticrew M, Roberts H. Evidence, hierarchies, and typologies: horses for courses. J Epidemiol Community Health, 2003,57:527-9.
- World Cancer Research Fund and American Institute for Cancer Research. Policy and Action for Cancer Prevention. Food, Nutrition, and Physical Activity: a Global Perspective. Washington, DC, 2009.
- Pawson R, Greenhalgh T, Harvey G, et al. Realist review - A new method of systematic review designed for complex policy interventions. Journal of Health Services Research and Policy, 2005,10:21-34.
- Rychetnik L, Frommer M, Hawe P, et al. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health, 2002,56:119-27.
- Rychetnik L, Wise M. Advocating evidence-based health promotion: reflections and a way forward. Health Promot Int, 2004,19:247-57.
- Bowen S, Zwi AB. Pathways to "Evidence-Informed" Policy and Practice: A Framework for Action. PLoS Medicine, 2005,2:600-05.
- Dobrow MJ, Goel V, Lemieux-Charles L, et al. The impact of context on evidence utilization: A framework for expert groups developing health policy recommendations. Social Science and Medicine, 2006,63:1811-24.
- The White House. Office of the First Lady. First Lady Michelle Obama Launches Let's Move: America's Move to Raise a Healthier Generation of Kids. http://www.whitehouse.gov/the-press-office/first-lady-michelle-obama-launches-lets-move-americas-move-raise-a-healthier-genera, February 9, 2010.
- Cohen L, Bell J. Letter to the Honorable Kathleen Sebelius, Secretary, U.S. Department of Health and Human Services. April 26, 2010 Available from: http://www.convergencepartnership.org/atf/cf/%7B245A9B44-6DED-4ABD-A392-AE583809E350%7D/PI-PL_input_on_PPH_Fund_doc-6.2.10.pdf, 2010.
- Braveman PA, Egerter SA, Woolf SH, et al. When do we know enough to recommend action on the social determinants of health? Am J Prev Med, 2011,40:S58-66.
- Brennan LK, Castro S. Exploring new opportunities for evidence-based decision making. Am J Prev Med, 2010,39:282-4.
- Cheadle A, Samuels SE, Rauzon S, et al. Approaches to measuring the extent and impact of environmental change in three California community-level obesity prevention initiatives. Am J Public Health, 2010,100:2129-36.
- Cheadle A, Schwartz PM, Rauzon S, et al. The Kaiser Permanente Community Health Initiative: overview and evaluation design. Am J Public Health,100:2111-3.
- Hiatt RA. Invited commentary: The epicenter of translational science. Am J Epidemiol, 2010,172:525-7; discussion 28-9.
- National Collaborative on Childhood Obesity Research. National Collaborative on Childhood Obesity Research, 2009. (http://www.nccor.org/).
- Caraher M, Coveney J. Public health nutrition and food policy. Public Health Nutr, 2004,7:591-8.
- Cummins S, Macintyre S. "Food deserts"--evidence and assumption in health policy making. BMJ, 2002,325:436-8.
- Heng HH. The conflict between complex systems and reductionism. JAMA, 2008,300:1580-1.
- Brunner E, Rayner M, Thorogood M, et al. Making Public Health Nutrition relevant to evidence-based action. Public Health Nutr, 2001,4:1297-9.
Acknowledgement and request
Readers are invited please to respond. Please use the response facility below. Readers may make use of the material in this editorial if acknowledgement is given to the Association, and WN is cited
Please cite as: Kumanyika S, Economos C Prevention of obesity. Finding the best evidence. [Commentary] World Nutrition, June 2011, 2, 6: 283-299. Obtainable at www.wphna.org
The opinions expressed in all contributions to the website of the World Public Health Nutrition Association (the Association) including its journal World Nutrition, are those of their authors. They should not be taken to be the view or policy of the Association, or of any of its affiliated or associated bodies, unless this is explicitly stated.
This commentary draws on the Institute of Medicine report, Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making, which was supported in part by Kaiser Permanente, the Robert Wood Johnson Foundation, and the US Centers for Disease Control and Prevention. The report was prepared by a committee composed of David Abrams, Ross Brownson, Frank Chaloupka, Madhabi Chatterji, Barbara Dennison, Steven Gortmaker, Lawrence Green, Robert Hiatt, William Purcell, Robert Sege, Harold Sox, Adolfo Valadez, Leticia Van De Putte, and Stephen West and the authors of this article, with the assistance of the following IOM staff: Lynn Parker, Leslie J. Sim, Emily Ann Miller, and Matthew Spear. Any views not attributed to the report are those of the authors and do not necessarily represent the views of the Institute of Medicine. SK is the main author of this commentary. It was initially drafted by her, incorporating key points from CE, and was subsequently reviewed and revised by the authors and by LJS, one of the IOM staff who was an editor of the report. No financial support was provided for the development of this commentary and the authors have no competing interests to declare.
WN commentaries are subject to internal review by members of the editorial team.